|
Abstract
Tuberculosis of the tongue is a very rare event even in areas and countries in which tuberculosis is endemic. The disease can present itself in a variety of clinical appearances, most of which may mimic malignant lingual neoplasms clinically. In this case, we present a patient who initially complained of an ulcerated lingual swelling, which was suspected to be a squamous cell carcinoma on clinical examination. In addition, the diagnosis was missed on the first and initial biopsy as it was not representative of the lesion. The diagnosis of lingual tuberculosis was made by histopathology on a second biopsy. In this article, we described the clinicopathological features of tuberculous glossitis with a comparison between our case and other similar reported cases in addition to a literature review.
Keywords: Tongue; Tuberculosis; Glossitis.
Introduction
Tuberculosis of the tongue, whether primary or secondary, is quite a rare phenomenon. Cases of lingual tuberculosis were recognized as early as 1888,1 and were published as isolated case reports or case series.2-9 The clinical diagnosis is often very difficult if not impossible as it is rare to suspect that an ulcer, fissure or nodular mass in the tongue is tuberculous in origin. More often, the diagnosis is made either by fine needle aspiration cytology or histopathological examination of a representative biopsy from the lesion. We present the findings of a case of tuberculosis of the tongue in a 42 years old Yemeni male who is a resident in the Kingdom of Saudi Arabia.
Case Report
A 42-years old previously healthy Yemeni male presented at the King Khalid University Hospital with a history of a persistent and non-healing ulcer on the lateral aspect of his tongue and extending to the lingual lip. The tongue tissue beneath the described ulcer was irregular and nodular in shape. Chest X-ray together with laboratory tests including complete blood count, coagulation profile, urea and electrolytes, as well as renal and liver function tests were reported to be within normal limits. Serological tests for HBV, HCV, HIV and syphilis were negative. Because the patient was a heavy smoker and an alcoholic in addition to the presence of an ulcerated tongue mass lesion, an initial clinical diagnosis of squamous cell carcinoma of the tongue was made. A biopsy taken from the tip of the tongue was reported as showing mucosal hyperkeratosis with nonspecific chronic inflammatory changes possibly due to chronic irritation. As there was a strong clinical suspicion of a squamous cell carcinoma, a repeat biopsy from an area adjacent to the ulcer was done and the second biopsy showed numerous caseating epithelioid and giant cells granulomata, (Fig. 1) containing scanty acid fast bacilli. A final histopathological diagnosis of tuberculous glossitis was later made and was supported by a positive PPD test and Mycobacterial culture from a sputum specimen. The patient was started on antituberculous therapy and follow up showed good initial response.
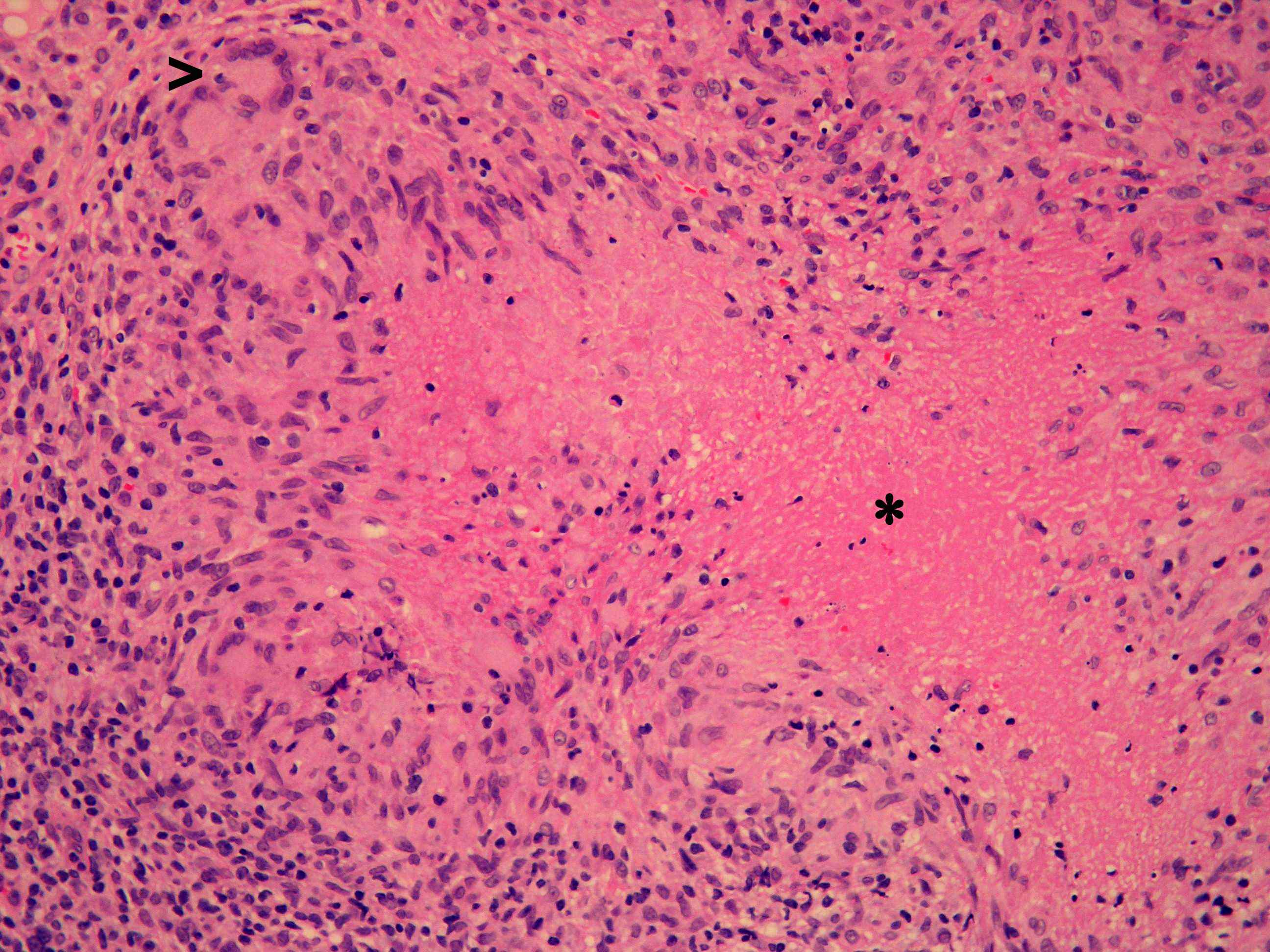
Figure 1: Primary tuberculosis of the tongue. A large epithelioid and giant cell granuloma (arrow head) and central caseous necrosis (asterix) are seen in this section which is taken from the tongue mass. Haematoxylin and eosin stain x 200.
Discussion
The World Health Organization (WHO) estimates that 2 billion people or one third of the world’s population are infected with tuberculous bacilli and the global tuberculosis incidence is growing at 1% a year.10 Despite these staggering figures, tuberculosis of the tongue is a rarely described entity with a rate of 0.1%.1-9,11 Furthermore, most cases of oral tuberculosis are mainly secondary to pulmonary tuberculosis and rarely primary in origin.2-7 Such lesions are suspected to be caused by implantation of infected sputum into a break in the mucosal surface during coughing episodes. Transmission during dental practice has also been described.12
Most authorities believe that the rarity of oral tuberculosis is due to the continuous cleansing of the oral mucosa by saliva, the presence of a variable normal flora in addition to the presence of submucosal antibodies which gives the buccal mucosa a normal resistance.8
Furthermore, the tongue does not contain any significant lymphoid tissue for which mycobacterium tuberculosis organisms has a great affinity.6,13 All these factors, relatively inhibit the growth of mycobacteria in the oral mucosa in general and the tongue in particular.3 Tuberculosis of the tongue almost always presents as a chronic non healing ulcer.3-11 Although the tongue is the commonest site for oral tuberculous lesions, they may also occur on the gingiva, floor of mouth, palate, lips and buccal mucosa.14
The current case differs from previously reported cases because the patient presented with a nodular and tumor-like mass which was clinically mistaken for a squamous cell carcinoma of the oral mucosa. This case also highlights the need to take deep biopsies from the edge of ulcerated lesions in order to avoid misdiagnosis due to non-representative biopsies which could be interpreted (as in the first biopsy obtained from this patient) as non-specific chronic inflammation.
The differential diagnosis of indurated tongue ulcers includes oral cancer (squamous cell carcinoma), lymphoma, salivary gland tumors and metastatic deposits. Other non-neoplastic differentials are traumatic ulcerations, aphthous ulcers and certain infections (such as primary syphilis, histoplasmosis and blastomycosis). The histopathological differential diagnosis includes other orofacial granulomatous conditions such as sarcoid, Crohn’s disease, deep mycoses, cat-scratch disease, foreign-body reactions, tertiary syphilis and Melkersson-Rosenthal syndrome. A detailed clinical history and examination are important to make up the diagnosis, ancillary studies including laboratory tests and radiological images are helpful although the tissue biopsy remains the golden standard for confirmation of the diagnosis.
Conclusion
In patients presenting with non-healing tongue ulcers associated with a nodular mass, the possibility of tuberculous glossitis should be included in the differential diagnosis and confirmed by histopathological examination of a representative and "deep tissue" biopsy.
Acknowledgements
The technical assistance of Mrs. Einam Gismalla during the processing and special staining of this case is greatly appreciated by the authors who also would like to thank Ms. Vivian Darusin.
|