|
A 55 years old male, a chronic smoker and a known diabetic was presented to the outpatient department, Sultan Qaboos University Hospital with complaints of change in voice, difficulty in swallowing and breathing for one month duration. The patient had minimal inspiratory stridor and flexible laryngoscopy showed a slough covered proliferative growth involving both surface of epiglottis and false cords, (Fig. 1). The vocal cords were mobile. The laryngeal crepitus was present and no neck nodes were clinically palpable. The patient denied any history of fever or weight loss. His total leukocyte count was normal; ESR was raised 48 mm 1st hour. The chest X-ray was normal and CT scan of the neck showed a contrast enhancing destructive lesion involving both surfaces of epiglottis and false cords. The patient was taken up for direct laryngoscopy and biopsy under general anaesthesia. There was minimal bleeding during the biopsy and there were no postoperative complications. The histopathology showed features of epitheloid granuloma, caseating necrosis surrounded by Langhans giant cells, (Fig. 2). The AFB stain and PAS stain for fungi were negative. Three specimens of sputum for acid fast bacilli were negative but the Monteux test was positive 15X15 mm.
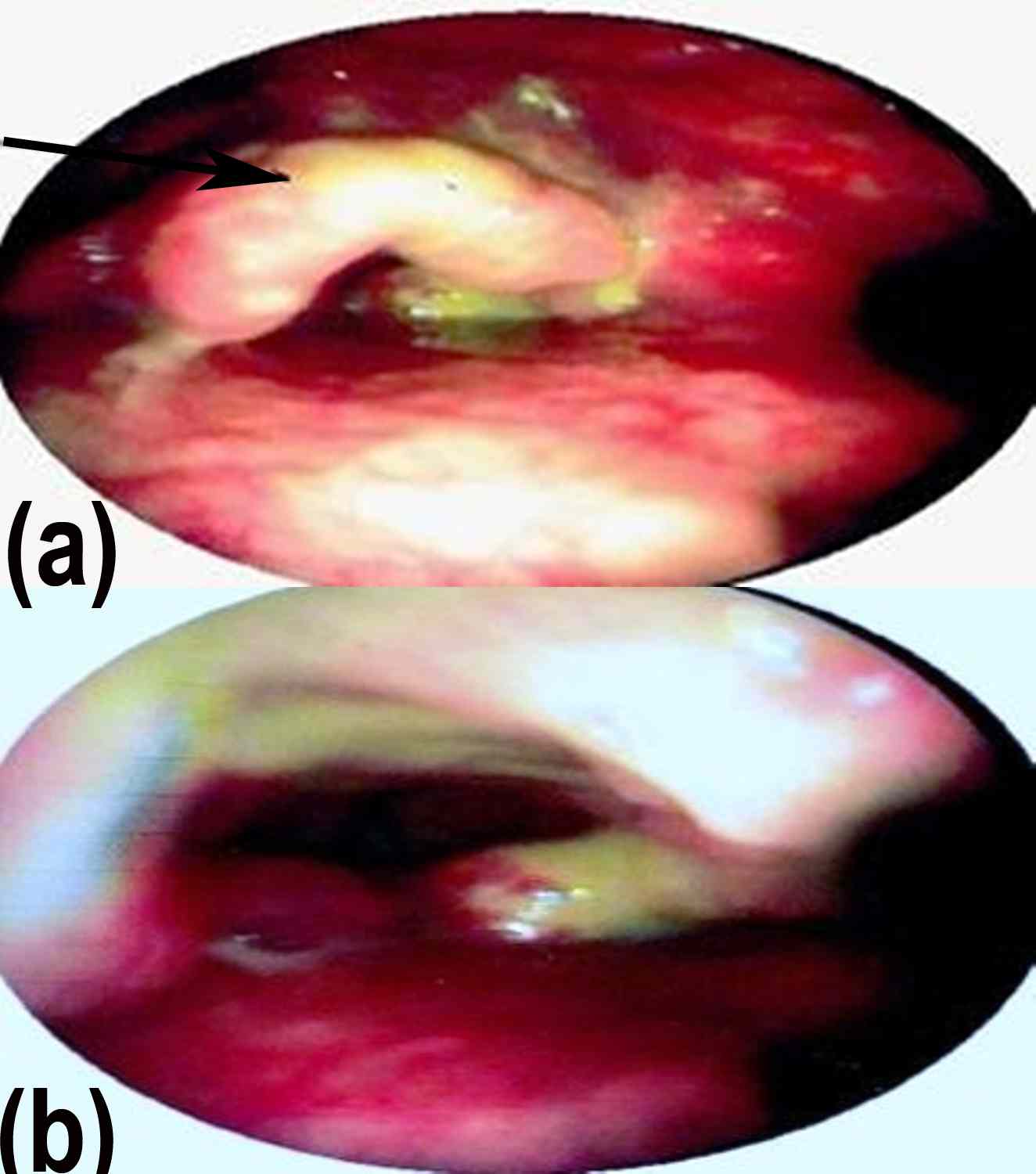
Figure 1: Clinical photograph showing (a) slough covered proliferative growth involving both surface of epiglottis (black arrow) and (b) false cords.
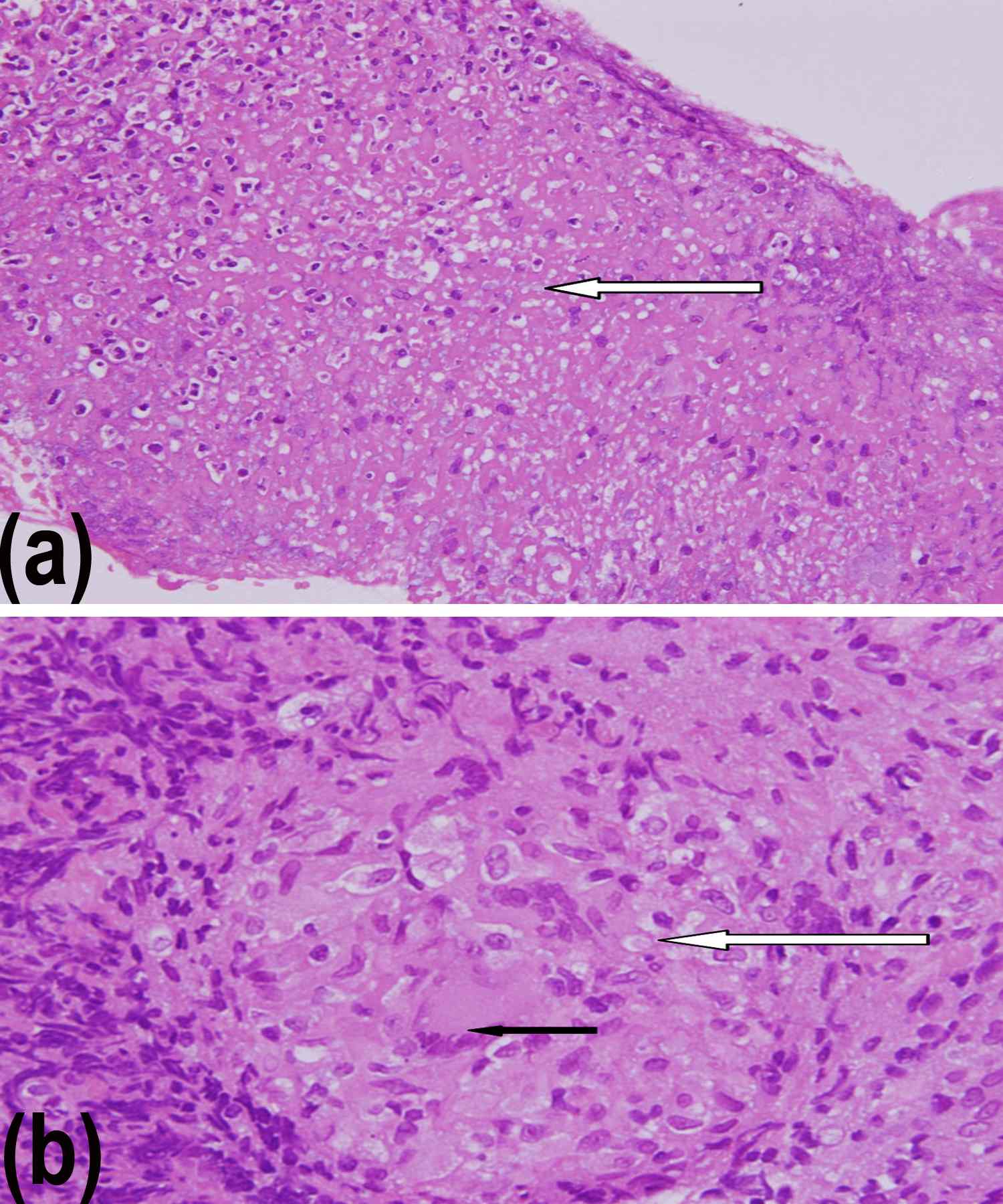
Figure2: Microphotograph showing; (a) central caesating necrosis {white arrow} H&EX40. (b) Epitheloid granulaoma {white arrow} and Langhans giant cells {black arrow} H&EX40.
Questions
1. What are the differential diagnoses of this case?
2. How should this patient be managed?
Answers
1. The differential diagnoses are laryngeal malignancy, chronic granulomatous pathology of larynx -tuberculosis, sarcoidosis and fungal laryngitis.
2. The histopathology is suggestive of tuberculosis in this patient. Patient requires anti-tubercular therapy as extra-pulmonary case and his family and close contact should be screened and treated accordingly.
Discussion
The clinical features of laryngeal tuberculosis (LT) and carcinoma overlap to a certain extent as both have similar presentation of hoarseness, dysphagia, dyspnoea and sore throat.1,2 Both cases are associated with history of weight loss, smoking and alcohol abuse.3,4 Isolated laryngeal involvement in sarcoidosis is rare and diffuse, oedematous, pale lesions are seen in suprglottis.5 Fungal laryngitis is seen in immunocompromised patients where whitish plaques are seen over vocal cords.6
LT exists in two forms i.e. primary and secondary. Secondary form is more common and is as a result of active pulmonary infection or rarely from hematogenous spread.7 The primary form as seen in our case is through inhalation of bacilli. Sub-mucosal tubercles are formed at the site of inoculation, which later ulcerates in areas where epithelium is tightly attached, such as vocal cords, arytenoids and epiglottis. While in other areas where epithelium is a lax, granulations spread and the lesion becomes bulky, as in aryepiglottic fold.
In the larynx, vocal cords are most commonly involved (50-70%) while epiglottis is least affected. The most common clinical presentation of LT is hoarseness of voice, pulmonary and constitutional symptoms like hemoptysis, cough, fever and weight loss are rare.7 The clinical appearance of lesion can change from ulcerative lesion to proliferate lesion and can be mistaken as a malignant lesion.2
LT being highly contagious poses a threat not only to family members, but also to the healthcare team during the course of diagnosis. Therefore, a high index of suspicion should be kept in elderly immune-compromised patients with laryngeal lesions, thus an early diagnosis and initiation of anti-tubercular therapy can achieve cure.
Acknowledgements
The authors reported no conflict of interest and no funding was received on this work.
|