A 70-year-old woman was brought to the emergency department after being found unresponsive on the floor by her family. She was last seen normal six hours before presentation. Past medical history included uncontrolled type 2 diabetes mellitus, stage 3 chronic kidney disease, and hypertension. Clinical exam revealed; blood pressure 210/120 mmHg, pulse rate 80/minute, respiratory rate 18/minute, temperature 37 oC, and oxygen saturation 99% on room air. The patient was stuporous; opened her eyes to pain, localized to pain with both upper limbs and had no verbal response (Glasgow Coma Scale 8). Her gaze was midline and pupils were 4 mm equal and reactive to light. Cardiac, respiratory, and abdominal exams were unremarkable. Blood glucose was 12 mmol/L.
Computed tomography scan of the head showed no acute intracranial process. Magnetic resonance images of the brain are shown [Figure 1].
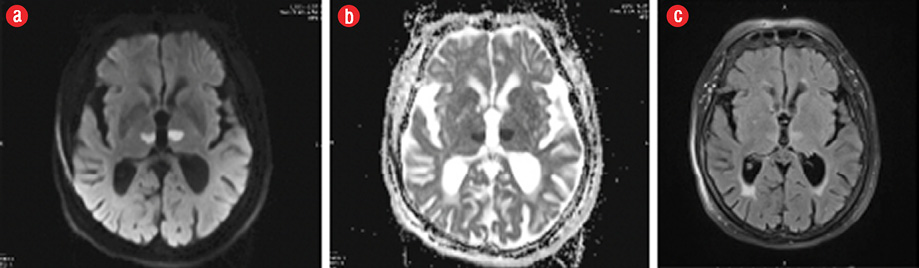
Figure 1: Patient's brain magnetic resonance imaging: (a) diffusion-weighted image. (b) apparent diffusion coefficient map, and (c) fluid attenuated inversion recovery sequence.
Question
- What is the diagnosis?
- Posterior reversible encephalopathy syndrome.
- Ischemic stroke.
- Osmotic demyelination.
- Deep cerebral venous thrombosis.
- Viral encephalitis.
Answer
b. Ischemic stroke.
Discussion
The patient had an acute ischemic stroke resulting in bilateral paramedian thalamic infarctions, consistent with artery of Percheron stroke.
The artery of Percheron is a rare anatomic variant of the posterior cerebral circulation in which a single unpaired thalamoperforating arterial trunk supplies blood to the paramedian thalami with or without extension to the rostral midbrain.1,2
Clinical presentation is variable; most patients present with impaired consciousness, hypersomnolence, amnesia, dysarthria, and ocular symptoms including vertical gaze palsy.2,3 Differential diagnoses include; top of the basilar syndrome, deep cerebral venous thrombosis, osmotic demyelination, Wernicke encephalopathy, viral encephalitis and toxic and metabolic encephalopathies.2
Diagnosis at presentation is challenging and requires high index of suspicion, so that time-sensitive treatment, such as fibrinolytic therapy, is instituted for patients who are candidates for such therapy and similarly unnecessary tests are avoided.
Disclosure
The authors declared no conflicts of interest.
references
- Lazzaro NA, Wright B, Castillo M, Fischbein NJ, Glastonbury CM, Hildenbrand PG, et al. Artery of percheron infarction: imaging patterns and clinical spectrum. AJNR Am J Neuroradiol 2010 Aug;31(7):1283-1289.
- 2. Vinod KV, Kaaviya R, Arpita B. Artery of Percheron Infarction. Ann Neurosci 2016 Jul;23(2):124-126.
- 3. Kumral E, Evyapan D, Balkir K, Kutluhan S. Bilateral thalamic infarction. Clinical, etiological and MRI correlates. Acta Neurol Scand 2001 Jan;103(1):35-42.