A 20-year-old woman with fever (39 °C) and chill was referred to our emergency department. She had noticeable jaundice and scleral icterus. She also reported a two-day history of epigastric pain radiating to the right upper quadrant, a mild sore throat, and urine discoloration. In the primary laboratory findings, elevated liver enzymes were detected, and abdominal sonography showed splenomegaly (131 mm) and gallbladder wall thickening (9 mm). Based on the clinical, laboratory, and imaging findings, the diagnosis of acalculous cholecystitis was made. For further evaluation, a complete serology test for viral and autoimmune hepatitis was required, which were all negative. Subsequently, the detection of immunoglobulin M (IgM) viral capsid antigen (VCA) Epstein-Barr virus (EBV) antibody and IgM cytomegalovirus (CMV) antibody was required. Based on the fever and abdominal pain, meropenem at a dose of 1 g three-times-daily was administered to the patient until the result of the laboratory test report. After one day, a generalized maculopapular rash developed on her face and spread to all parts of the body. Treatment was discontinued [Figure 1].
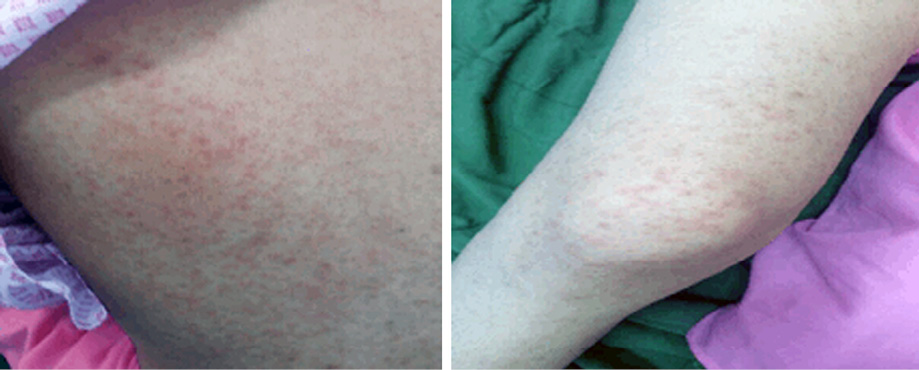
Figure 1: Generalized maculopapular rash induced by meropenem.
The rash disappeared gradually after discontinuation of meropenem. The patient was not penicillin-sensitive and had no history in this regard. IgM VCA (EBV) antibody was positive. Hence, the diagnosis of acalculous cholecystitis due to EBV was confirmed, and supportive care without surgery was considered. The Naranjo scale showed a probable association between meropenem usage and rash occurrence. It is recognized that skin rash may develop during acute EBV. These rashes are mostly maculopapular exanthems or morbilliform, which appear on the whole body, even though in severe cases, it turns into erythroderma. Viral infections also may lead to skin eruption. However, viral infection is a risk factor for developing drug allergic reactions.1,2 The underlying mechanism of drug eruption in this patient may be explained by two different pathways. The first hypothesis described this eruption as a penicillin hypersensitivity phenomenon, where penicillin polymer-mediated lymphocyte stimulation has an important role in the development of maculopapular rash.3,4 The second mechanism described a non-immunological reaction because such eruptions did not appear after drug re-challenge. In this regard, some antibodies in both IgM and IgG immunoglobulin classes have activity against penicillin. In some situations, with elevated levels of IgM and IgG (e.g., EBV), penicillin could have an interaction with these antibodies. Hence, the observed rash in the current patients may be a consequence of complement system activation, which was associated with circulating antigen-antibody complexes.5 This adverse drug reaction with meropenem is a novel case that may be associated with EBV infection. This case emphasizes the increased probability of drug eruption in EBV patients. Hence, physicians must be aware of the risk of drug eruptions in such patients and appropriate strategies must be predicted before administering antibiotics.
references
- 1. Dibek Misirlioglu E, Guvenir H, Ozkaya Parlakay A, Toyran M, Tezer H, Catak AI, et al. Incidence of antibiotic-related rash in children with Epstein Barr virus infection and evaluation of the frequency of confirmed antibiotic heypersensitivity. Int Arch Allergy Immunol 2018;176(1):33-38.
- 2. Al-Raaie F, Banodkar DD. Epidemiological study of cutaneous adverse drug reactions in Oman. Oman Med J 2008 Jan;23(1):21-27.
- 3. Hanto DW, Frizzera G, Purtilo DT, Sakamoto K, Sullivan JL, Saemundsen AK, et al. Clinical spectrum of lymphoproliferative disorders in renal transplant recipients and evidence for the role of Epstein-Barr virus. Cancer Res 1981;41(11 Pt 1):4253-4261.
- 4. Roujeau JC. Immune mechanisms in drug allergy. Allergol Int 2006 Mar;55(1):27-33.
- 5. Hochberg D, Souza T, Catalina M, Sullivan JL, Luzuriaga K, Thorley-Lawson DA. Acute infection with Epstein-Barr virus targets and overwhelms the peripheral memory B-cell compartment with resting, latently infected cells. J Virol 2004 May;78(10):5194-5204.