Insulin resistance syndrome includes a large variety of diseases; metabolic syndrome is the most common disease and is associated with obesity, glucose intolerance, and diabetes. However, severe insulin-resistant states are rare and are reported in genetic, immunological, and endocrine diseases. Individuals with severe insulin resistance syndrome present with a cluster of related abnormalities that are classified into different phenotypes.1 Type A insulin resistance is a rare autosomal-dominant mutation of the insulin receptor (IR).2 On the contrary, type B insulin resistance is defined as an autoimmune condition where polyclonal immunoglobulin G antibodies act directly against IRs and is characterized by extreme insulin resistance, uncontrolled diabetes (even with massive doses of insulin), significant weight loss, severe hyperandrogenism in women, and unusually widespread acanthosis nigricans (AN).3
Type B insulin resistance syndrome (TBIRS) usually presents with features of other autoimmune diseases in association with a common presentation of severe insulin resistance.1,3 The presence of anti-IR antibodies in the plasma is the diagnostic hallmark of this syndrome. Other nonspecific laboratory findings for this syndrome include elevated erythrocyte sedimentation rate, leukopenia, hypergammaglobulinemia, presence of serum antinuclear antibodies (ANA), and proteinuria.1,3 Various therapeutic approaches for TBIRS have been attempted, which show different responses. These include a variety of steroid preparations, plasmapheresis, azathioprine, mycophenolate mofetil, cyclophosphamide, and rituximab.4
This syndrome has been rarely reported in deferent ethnicities and has not yet been reported in Arabs. Therefore, this case describes the first middle-aged African Arab male patient who was diagnosed with TBIRS associated with mixed connective tissue disease (MCTD).
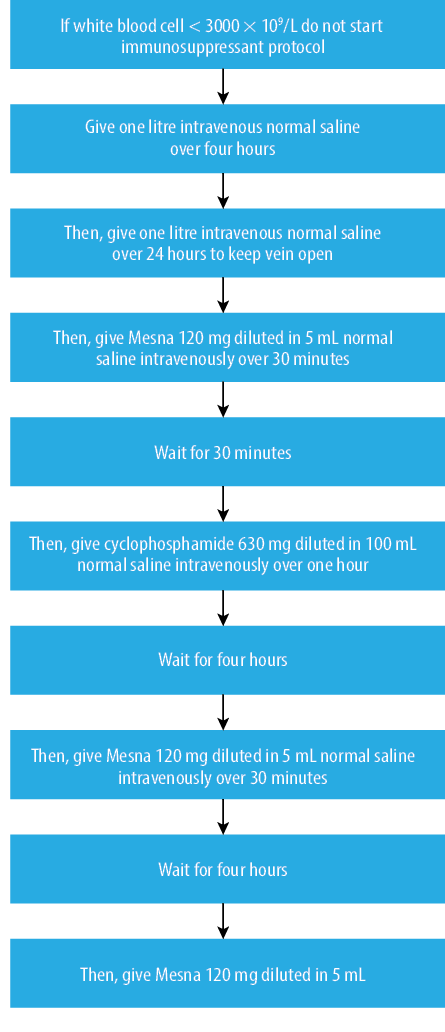
Figure 1: Immunosuppressant protocol used to treat patient’s type B insulin resistance syndrome.

Figure 2: (a) Blood sugar profile before management. (b) Blood sugar profile after immunotherapy and plasmapheresis with complete normalization of blood sugar levels.
Case report
A 38-year-old Sudanese man was diagnosed with type 2 diabetes using the American Diabetic Association criteria with significant hyperglycemia seven years prior to his presentation. He was started on diet and exercise. He responded well and exhibited normal glycated hemoglobin (HbA1c) levels. Three years later, symptoms such as polyuria and polydipsia increased in severity as his blood glucose levels increased. Glimepiride was started at a dose of 3 mg administered once daily in addition to metformin (850 mg three times daily), which controlled his blood sugar for the next two years.
Upon initial presentation, the patient complained of generalized joint pain and severe hyperglycemia despite being managed with 200 units of regular human insulin (U100) every four hours in addition to pioglitazone (30 mg administered once daily) and metformin (850 mg administered three-times daily). The patient experienced weight loss
(~ 40 kg) within four months. He had significantly high titers of ANA, rheumatoid factor (RF), and ribonucleoprotein (RNP). He was also diagnosed with MCTD by a rheumatologist at another hospital. The patient was initially treated with methotrexate (10 mg/week) for a short period, which was replaced by hydroxychloroquine (200 mg/day). Previous investigations also showed a decreased white blood cell count, negative insulin antibodies, positive IR antibodies, and decreased leptin and insulin-like growth factor-1 (IGF1) levels, which suggest severe insulin resistance.
His vital signs were normal, with a pulse of 78 beats per minute and blood pressure of 120/80 mmHg. His weight was 74.7 kg, height was 181 cm, and body mass index (BMI) was 22.8 kg/m2. He had severe AN at the back of the neck and axillae.
His initial laboratory tests demonstrated leukopenia with normal liver and kidney functions, but negative serology for HIV 1 and 2. His triglyceride level was relatively low (0.72 mmol/L) with a triglyceride/high-density lipoprotein ratio of 0.26, but other lipid profile parameters were normal. His HbA1c was 12.9% and average blood sugar readings ranged from 22.2 mmol/L (400 mg/dL) to 27.8 mmol/L (500 mg/dL). His detailed immunological workup revealed positive antibodies for RNP (318 IU/mL), IR, ANA (1:320), and RF. He tested negative to insulin, double-stranded DNA, anti-microsomal, and anti-thyroid antibodies. He had normal thyroid functions, cortisol levels (441 nmol/L), and growth hormone levels (0.6 ng/mL). In addition, the results of the computed tomography of the adrenal gland and magnetic resonance imaging of the pituitary were unremarkable.
Upon admission, he was managed as a type 2 diabetes mellitus patient who developed secondary failure to oral hypoglycemic agents. He was initially treated with 100 units of glargine twice daily, 8 mg of rosiglitazone once daily, and 160 units of insulin aspart administered subcutaneously every two hours. Based on his total insulin daily dose, he was categorized as extremely insulin resistant. Other endocrine diseases, mainly Cushing’s syndrome and acromegaly, which could be the reason for his presentation, were ruled out. The patient was diagnosed with TBIRS after confirming the presence of MCTD and positive anti-IR antibodies.
Based on the assessment of the rheumatology team, the patient was started on intensive cyclophosphamide pulses along with plasmapheresis, which were performed according to the management protocol [Figure 1]. He received high doses of prednisolone (40 mg twice daily) and was on continuous hydroxychloroquine treatment. During the course of his treatment, he was closely monitored using a continuous glucose monitoring system, which showed marked improvement in the blood sugar pattern [Figure 2]. After completing two courses of pulse cyclophosphamide therapy along with three sessions of plasmapheresis over the next three months, his HbA1c decreased from 12.9% to 7.3%. His insulin requirement reduced from an initial total dose of 1200 units per day to 32 units per day. His prednisolone dose was also reduced from 40 mg twice daily to 20 mg twice daily. Moreover, he gained 9 kg in weight, and his BMI increased from 22.8 kg/m2 to 25.5 kg/m2.
During the treatment course, he developed a few consequent complications such as fever and a gluteal abscess, which were managed surgically and medically with oxacillin IV 500 mg twice daily and metronidazole IV 500 mg three times daily. After recovery from the gluteal abscess, he developed left lower lobe pneumonia and was treated with Tazocin (piperacillin/tazobactam) 4.5 g IV every four hours and azithromycin 500 mg IV once daily, based on the culture results. During these episodes of acute infection, he developed diabetic ketoacidosis and was managed successfully and uneventfully with intravenous insulin aspart at a dose of 200 units per hour. After the infection subsided, he had episodes of hypoglycemia. Hence, the insulin dose was reduced and eventually stopped for a few days. He later developed hyperglycemia, and glargine insulin was resumed at a dose of 30 units once daily, along with insulin aspart at a dose of 15 units three times daily, which were reduced gradually.
Table 1: Patient’s laboratory results upon admission and discharge.
|
WBC |
2.2 × 109/L |
4.1 × 109/L |
|
Neutrophil count |
0.84 × 109/L |
2.6 × 109/L |
|
ESR |
65 mm/hr |
20 mm/hr |
|
CRP |
201 mg/L |
6 mg/L |
|
HbA1c |
12.9% |
7.3% |
|
Insulin |
148.6 IU/mL |
14.65 IU/mL |
WBC: white blood cell; ESR: erythrocyte sedimentation rate; CRP: C-reactive protein; HbA1c: glycated hemoglobin.
He was discharged on prednisolone 20 mg once daily, hydroxychloroquine 200 mg once daily, and 20 units of glargine once daily along with 4 units of insulin aspart administered three-times daily. Upon discharge, improvements in glycemic, inflammatory, and immunity parameters were noted [Table 1]. Within his four months of hospital stay, he showed dramatic improvements in glycemic control, insulin requirement, weight gain, joint pain, and general well-being [Figure 3].

Figure 3: Management protocol used to treat this patient with normalization of blood sugar levels
and cessation of insulin therapy as outcomes of
the management.
He was followed-up in the outpatient clinic on a monthly basis. Over the next six months of follow-up, the doses of prednisolone, insulin, and rosiglitazone were gradually decreased and eventually discontinued. Moreover, his HbA1c decreased from 7.3% to 5.6%, his average blood sugar level was 8.3 mmol/L (150 mg/dL) [Figure 3], and his weight reached 100 kg. He was kept under hydroxychloroquine therapy and showed good progress without any antidiabetic treatment.
Discussion
We report an important but unusual case of TBIRS. This is the first case reported among Arabs with African descent. African Americans are the group most susceptible to TBIRS, followed by Asians, which represents almost one-fifth of all cases. TBIRS is usually associated with systemic lupus erythematosus (SLE), mainly in women.5 MCTD was associated with TBIRS in a few reported cases.4,6 This is the first case report to evaluate the association between MCTD and TBIRS among Arabs with African descent.
We conducted a literature review and found no specific criteria to diagnose TBIRS. However, some cardinal clinical and biochemical features can be used to diagnose this condition. The biochemical triad of elevated fasting insulin concentrations, hyperadiponectinemia, and low/normal fasting triglyceride concentrations in an individual with AN point toward the diagnosis. The presence of autoimmune disease, either SLE or MCTD, suggests TBIRS, along with the presence of anti-IR antibodies. This case has had most of the clinical and biochemical findings that would suggest the syndrome, in addition to significant weight loss indicating catabolic phase related to severe insulin resistance.4
This case demonstrated the difficulties in the management of patients with severe insulin resistance or conditions that involve autoimmunity. Similar to what has been previously reported by other cases,4,7 diabetic ketoacidosis reported in this case was also associated with precipitating factors (gluteal abscess) although leukopenia is expected in such clinical conditions. It can also be explained by stress-induced ketoacidosis and/or severe catabolic state in such cases. Administration of immunosuppressive agents may reduce the patient’s immunity, and this is usually associated with increased risk of infection.4 In this report, the patient developed recurrent hypoglycemia when the IR antibody titer was suppressed either by plasmapheresis or treatment with immunosuppressive agents. Previous studies have reported that high titers of this antibody act as an antagonist at the receptor level. At low titers, it acts as an agonist, resulting in different degrees of hyperglycemia and/or hypoglycemia.5
Although there is no standardized method for the management of TBIRS cases, several therapeutic regimens have been attempted with different rates of success. However, the management of such cases should focus on two parameters: the catabolic state that patients present with and the autoimmune process, which is the main cause of the disease.8 Our patient was initially managed with high doses of insulin (up to 4800 units/day) to restrain the catabolic state rather than achieving normoglycemia, which is usually attained by immunotherapy.
A variety of immunosuppressive agents, including glucocorticoids, cyclophosphamide, and azathioprine, cyclosporine, rituximab, mycophenolate mofetil, and intravenous immunoglobulin, have been reported to induce remission either alone or in combination.4,6,8,9 Plasmapheresis was performed with various responses and was recommended for patients with very high titers of IR autoantibodies.8–10 In poorly responsive cases to combination therapy of glucocorticoids and other immunosuppressive agents, standardized treatment with rituximab, cyclophosphamide, and pulse steroids result in remission of the disease.7 Our patient was successfully treated with an intensive pulsed combination regimen of cyclophosphamide, prednisolone, and plasmapheresis. MCTD was managed with hydroxychloroquine to which the patient had a good response. The patient’s treatment response was monitored and showed a decrease in HbA1c from 12.9% to 5.6%, weight gain from 74.7 kg to 100 kg, and a highly significant decrease in insulin requirement, from around 2000 units per day to none.
The prognosis of TBIRS is divided into three categories: one-third of the cases will have spontaneous remission, another one-third will have remission in response to the therapy, and the remaining third will not achieve remission even with treatment. Time to remission is reported to be inconsistent, ranging from six months to two years, and our patient achieved remission within four months.7 The recurrence rate remained unknown; however, the mortality rate was as high as 50% within 10 years of diagnosis.3
Conclusion
An Arab male patient had a severe form of TBIRS complicated by severe hyperglycemia, diabetic ketoacidosis, and leukopenia and was successfully managed with immunosuppressive agents and plasmapheresis. He fully recovered from insulin resistance and exhibited normal metabolic status.
Disclosure
The authors declared no conflicts of interest.
references
- 1. Mantzoros CS, Flier JS. Insulin resistance: the clinical spectrum. Adv Endocrinol Metab 1995;6:193-232.
- 2. Semple RK, Williams RM, Dunger DB. What is the best management strategy for patients with severe insulin resistance? Clin Endocrinol (Oxf) 2010 Sep;73(3):286-290.
- 3. Arioglu E, Andewelt A, Diabo C, Bell M, Taylor SI, Gorden P. Clinical course of the syndrome of autoantibodies to the insulin receptor (type B insulin resistance): a 28-year perspective. Medicine (Baltimore) 2002 Mar;81(2):87-100.
- 4. Malek R, Chong AY, Lupsa BC, Lungu AO, Cochran EK, Soos MA, et al. Treatment of type B insulin resistance: a novel approach to reduce insulin receptor autoantibodies. J Clin Endocrinol Metab 2010 Aug;95(8):3641-3647.
- 5. Buhaescu I, Rhee S, York MR, McDonnell M, Merkel PA. A woman with severe lupus nephritis and difficult to control diabetes mellitus. Arthritis Care Res (Hoboken) 2011 Apr;63(4):623-629.
- 6. Yang H, Zhao J, Li Y, Lv F, Zhang S, Li Y. Successful treatment of type B insulin resistance with mixed connective tissue disease by pulse glucocorticoids and cyclophosphamide. J Diabetes Investig 2017 Jul;8(4):626-628.
- 7. Robinson C, Cochran E, Gorden P, Brown RJ. Management of diabetic ketoacidosis in severe insulin resistance. Diabetes Care 2016 Aug;39(8):e116-e118.
- 8. Page KA, Dejardin S, Kahn CR, Kulkarni RN, Herold KC, Inzucchi SE. A patient with type B insulin resistance syndrome, responsive to immune therapy. Nat Clin Pract Endocrinol Metab 2007 Dec;3(12):835-840.
- 9. Zhang S, Wang G, Wang J. Type B insulin resistance syndrome induced by systemic lupus erythematosus and successfully treated with intravenous immunoglobulin: case report and systematic review. Clin Rheumatol 2013 Feb;32(2):181-188.
- 10. Eriksson JW, Bremell T, Eliasson B, Fowelin J, Fredriksson L, Yu ZW. Successful treatment with plasmapheresis, cyclophosphamide, and cyclosporin A in type B syndrome of insulin resistance. Case report. Diabetes Care 1998 Aug;21(8):1217-1220.