|
Abstract
Objective: To determine the pattern of headache and its associated symptoms in school going children.
Methods: The data of all the school going children attending the Headache Clinic in the Dept. of Neurology, Dhaka Medical College Hospital were retrospectively reviewed. A total of 1021 patients from October 1996 to September 2011 were selected. Data were collected through a predesigned questionnaire containing information on age, sex, social status, clinical features, opthalmoscopic findings, management, and in selected cases imaging results.
Result: The mean age of headache in school children was 12.6±1.08 years with relatively older age of presentation among girls. The sex ratio was 1.64:1 in favor of girls at older age. Tension type headache (71.1%) was the most common form of headache, followed by migraine (18.4%) and mixed headache (6.7%). Though the girls had more frequent headache of both tension type (59.4%) and migraine (68.1%) variety, the latter was significantly associated in girls (p<0.001). Headache was of moderate severity in 53.3%, whereas severe headache was experienced by 19.9% of the children. The children commonly had nausea and/or vomiting (47.2%), as well as photophobia (24.7%) with headache. Mentalstress (34%) and sunlight (30.9%) were common triggering factors whereas a sound sleep relieved headache in the majority (59.4%). Paracetamol (83.3%) and nor tryptyline (62.8%) were the most commonly prescribed drug taken by them.
Conclusion: Headache is a major health problem in school children, apart from other common health issues at this age. With increasing age, the girls more commonly suffer not only from migraine but also with other chronic headache. The direct causal association is yet to be determined.
Keywords: Headache; Tension type headache (TTH); migraine.
Introduction
Headache is the commonest neurological condition in terms of the number of people affected.1 It is also a common symptom and health problem among school children.2,3 Though, the overall prevalence of headache in children and youngsters is about 53% in developed countries, the life time prevalence in adult increases up to 77%.4 An epidemiologic survey of school children revealed that about one third of the children who were at least seven years of age and one half of those who were at least 15 years of age had repeated headache.5 Recurrent headaches can negatively impact a child’s life in several ways, including absence from school, decreased academic performance, social stigma, and impaired ability to establish and maintain peer relationships. The quality of life in a child with migraine gets impaired to an extent similar to cancer or arthritis.6
There is paucity of data on headache in school children, especially in Bangladesh. Most of the knowledge on this group of patients is based mainly on studies from European countries and few reports from the United States.7-10 Thus, this study was conducted on school-going children in a specialized out-patient Headache Clinic at Dhaka Medical College Hospital (DMCH) to get a glimpse of the problem among young students.
Methods
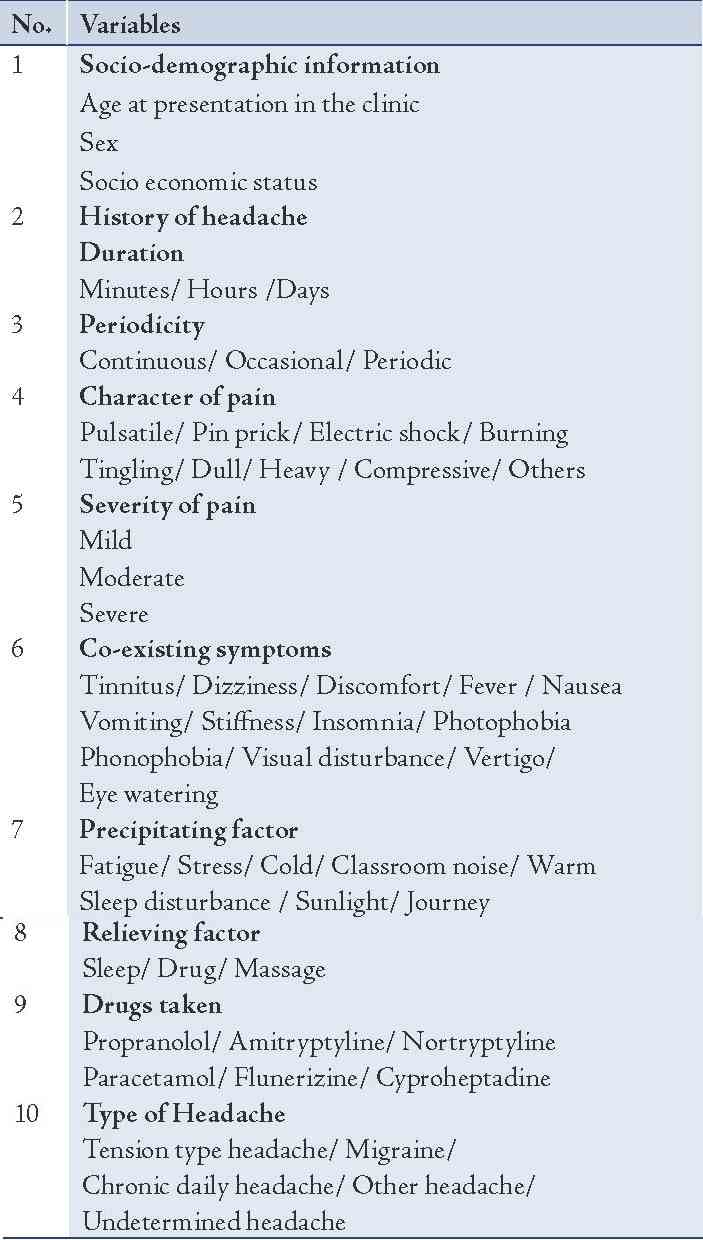
This is a retrospective study carried out in a weekly Headache out-patient clinic at the Department of Neurology, DMCH from October 1996 to September 2011. During this period, a total of 11,587 patients with headache disorders were seen at the Neurology OPD (out-patient department) of DMCH. A total of 1021 school children who were between 4 to 15 years of age with headache disorders were included for the study. A preformed questionnaire was used containing information on age, sex, social status, clinical features, opthalmoscopic findings, management and imaging studies. (Table 1)
The socioeconomic status of patients were categorized arbitrarily for the study into upper (>$600 per month), middle ($60 to $600 per month), and lower class (<$60 per month) in accordance with the monthly income of their parents. Patients were initially examined by research assistants. All of the research assistants who took part in the study were postgraduate resident trainees at the Neurology department. They were well trained by Professors of Neurology at DMCH. Each patient was later evaluated meticulously and treated by consultant neurologists working at the Headache Clinic. Diagnosis was made on clinical ground following the International Classification of Headache Disorder version 2 (ICHD-II) criteria at the clinic. Prior to 2004, the clinic used the first edition of classification system published in 1988. The clinical diagnosis was used as a gold standard, based on the experience of the consultant neurologists in headache diagnosis, the clinical features described by the patients and parents including the components discussed in ICHD-II criteria, and the supportive history including the family history of headache, response to treatment and records of previous headache. Headache disorders were broadly classified into five major groups namely; tension-type headache (TTH), migraine, chronic daily headache (CDH), and others. Those having very little information, allowing only the state of headache but not the type were regarded as unspecified/undetermined headache. The terms TTH and migraine were used according to the diagnostic criteria of ICHD-II. The clinical diagnosis of migraine as a primary diagnosis included all the subtypes (migraine with aura, migraine without aura, chronic migraine, and probable migraine). CDH was defined as primary headache occurring more than 15 days per month for more than 3 months in the absence of an organic pathology. Further subclassification of these major groups of headaches was avoided for the purpose of simplification of the study and minimization of any chance of diagnostic error. CT scan of head and other investigations were done only in selected cases.
Table 1: Variables recorded in the clinic questionnaire.
The research protocol of this study was approved by the institutional ethical committee at Dhaka Medical College. Data were collected from hospital records and analyzed using SPSS-16 system. Chi-square test was used to test the difference between categorical variables. A p-value less than 0.05 was considered significant, taking into account the confidence interval (CI) at 95%.
Results
Out of 11,587 patients seen in the Headache Clinic during the 15-year period, the samples for this study included 1021 students (8% of all headache patients), starting from Kindergarten at four years of age to 15 years old teenagers. Among them, 60.9% were girls and only 39.1% were boys. Though the sex ratio was 1:1 in children aged less than 5-years, and the number of girls was almost two thirds of all in the older age group, (Fig. 1). The frequency of migraine type of headache among girls was twice that of boys and the difference was highly significant (p<0.001), (Fig. 2). Majority of the children with headache in the study group were aged between 11 and 15 years (79.6%), (Table 2). The mean age at presentation was 12.6±1.08 years for all the children. The girls were relatively older at presentation to the Headache Clinic with a mean of 12.8±1.09, whereas the mean age at presentation was 12.1±1.06 for the boys. The children’s social status was also considered, and the major portion of them belonged to middle class families (72.4%). The rest (27.6%) had lower socioeconomic backgrounds, but none were from the higher class of social strata. (Table 2)
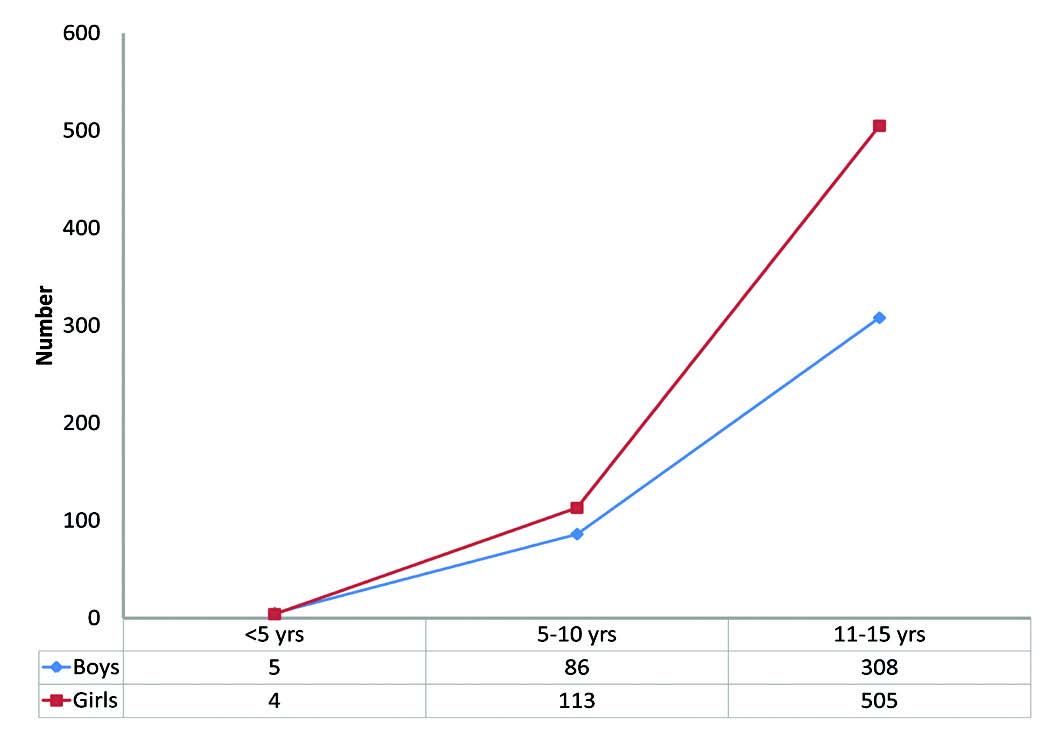
Figure 1: Age and Sex Distribution of patients.
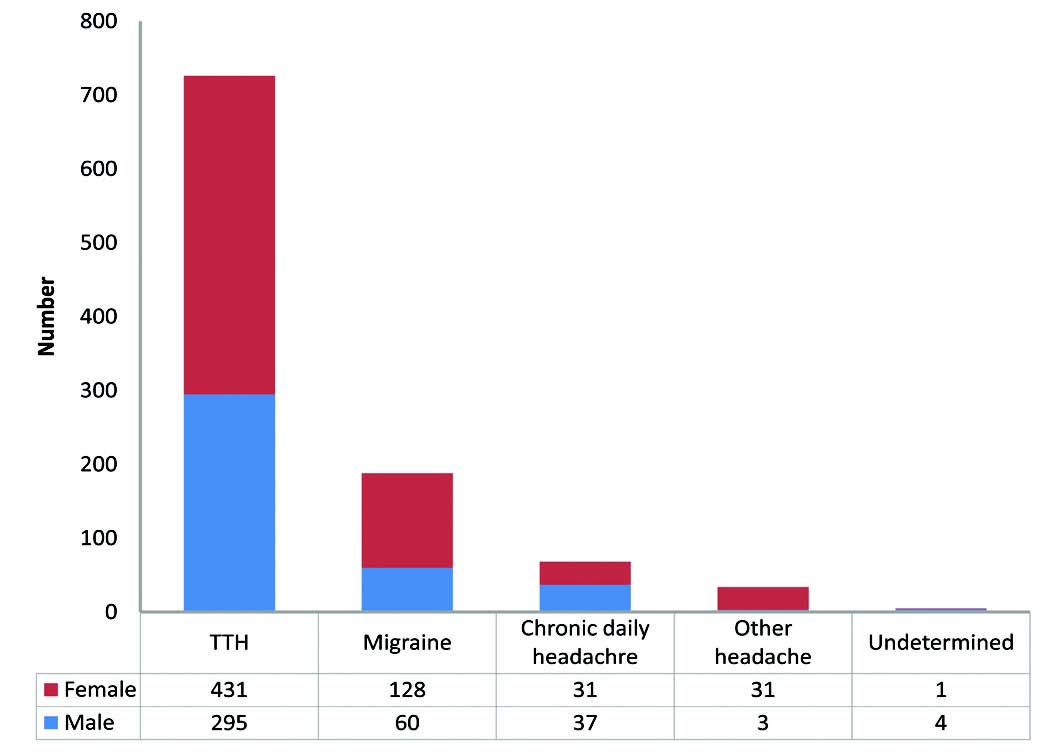
Figure 2: Distribution of different types of headache among both sexes.
Table 2: Socio demographic profile of the patients (N=1021).
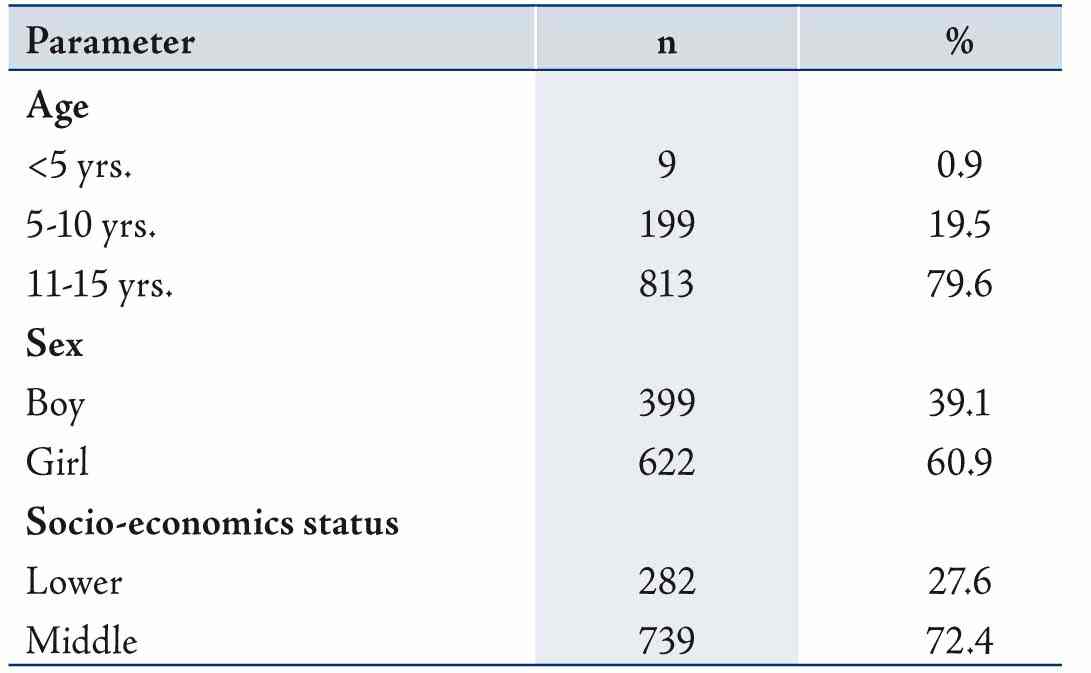
Table 3: Characteristics of Headache (N=1021).
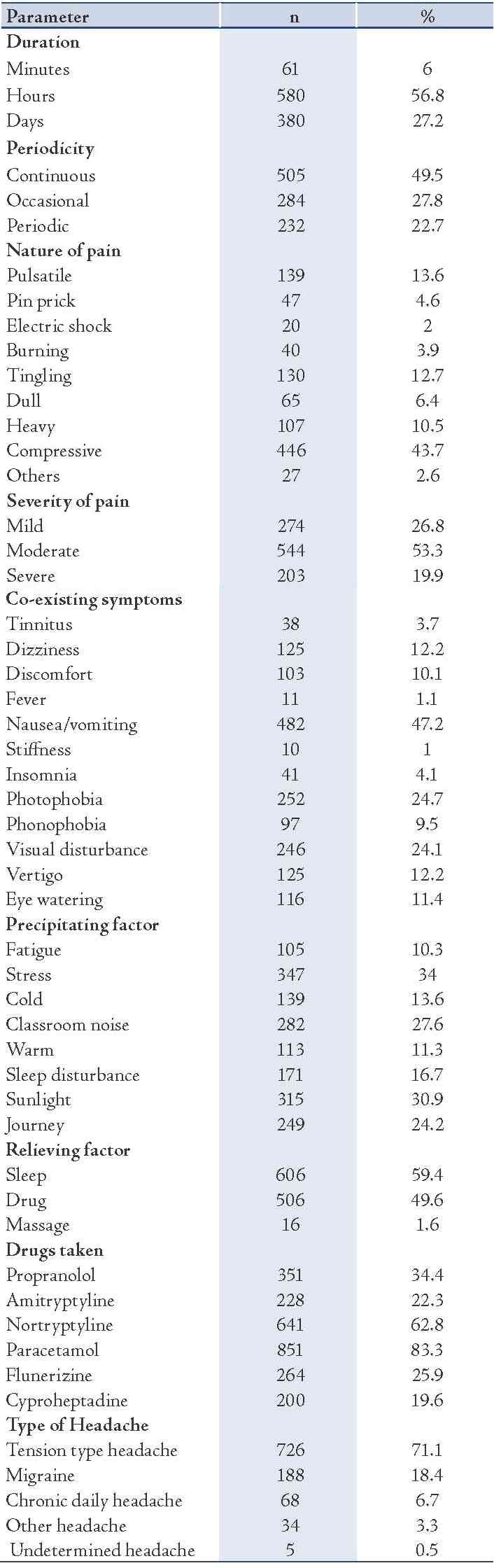
Table 3 shows the characteristic features of headache including symptomatology, different influencing factors, clinical findings and the treatment received by the patients.
The duration of an individual episode of headache varied considerably where headache persisted for hours in 56.8% of the students. Headache was continuous in most of the children (49.5%) and only 22.7% experienced headache periodically, (Table 3). The majority reported a compressive (446) nature of their headache, the rest had pulsatile (139), tingling (130), heaviness (107), dull (65) type of pain. Regarding the severity of headache, 53.3% had moderate, 26.8% had mild and 19.9% had severe pain. On the query of co-existing factors associated during an attack of headache, about half of the children (47.2%) reported nausea and or vomiting. Photophobia (24.7%), visual disturbance (24.1%), dizziness (12.2%), vertigo (12.2%), eye watering (11.4%) were also commonly reported. (Table 3)
Different physical and emotional stimuli like mental stress (34%), exposure to sunlight (30.9%), classroom noise (27.6%), journey (24.4%), sleep disturbance (16.7%), etc. precipitated headache episodes in many students. Sound sleep reduced the pain in most cases (59.4%), whereas many children got relief from headache after taking some medications (49.6%). Paracetamol (83.3%) and nortryptyline (62.8%) were most frequently prescribed by the physicians for childhood headache. Some students received propranolol (34.4%), amitryptyline (22.3%), flunarizine (25.9%), cyproheptadine (19.6%) in different combinations. (Table 3)
Among the different headache disorders, tension type of headache (71.1%) was most frequently encountered by these students, followed by migraine (18.4%), and chronic daily headache (6.7%). Other types of primary headache and causes of secondary headache were present only in small number of students (3.3%). Despite the extensive evaluation with the help proper history, clinical examination and imaging studies, as well as the type of headache were undetermined in five students. (Fig. 2)
Discussion
Most of the epidemiological studies on headache in school children are from Finland,11 Denmark,12,13 Sweden,14 United Kingdom,15,16 USA,17 and Australia.18 The prevalence of migraine and other headaches varies between 3% to 10% in these studies. Though not directly comparable to these studies due to difference in methodology, a headache frequency of 8% in school children was also found among all the headache patients attending the specialized outpatient hospital clinic. The prevalence estimate in pre-pubertal children ranged from 2.4% to 17% for migraine and 4% to 5% for other severe recurrent headache, which increases considerably in post pubertal period,5,7-11,18 but the rate of recurrent headache was also found to be higher (20% to 50%) in these countries.3,14,19,20 Though the distribution of migraine was similar in this study, the rate of common tension type recurrent headache was much higher (70.1%). Furthermore, cultural difference may play a substantial role. In general, somatization of different complaints often in the form of headache may reflect the common psychosocial behavior of children. Headache is an acceptable symptom especially to avoid the load of study and pressure of school among children.
A Finnish study reported an increasing trend of migraine over the last decade in children during the first few years of their schooling.21 The reason might lie in the improved headache classification criteria and increasing awareness among parents. The most common age of headache presentation in this study was similar to other studies in both developed and under developed countries. The sex ratio for headache was also not different from that of Lateef et al. in USA, where the girls with headache outnumbered the boys after the age 12.22 This may be due to the social and cultural restrictions imposed particularly on teenage girls. Kowal et al. showed that the social expectations of girls are different from boys, especially in the aspect of social freedom, choice and peer relation. This often becomes a source of internal conflict, anxiety and mood problems which frequently accompanies headache.23 Other headache characteristics (eg., duration, periodicity, severity and nature of pain, associated symptoms, precipitating and relieving factors, and medication used before specialist consultation) were also examined in this study. Distribution of these variables followed more or less a similar pattern to that of European studies and of developing countries like Pakistan.24,25
In compliance with the current knowledge and understanding of the basic pathophysiology of migraine, it was found that girls had migraine more frequently with increasing age than boys (p<0.001) in this study. Launer et al. and Molgard et al. showed that the prevalence of migraine increases after puberty in girls.26,27 During the reproductive years, there is also marked gender difference in prevalence and type of migraine. Migraine without aura is more common in women at their reproductive age.6,26,28,29 Due to the fact that patients from higher socioeconomic background usually visit private hospitals and specialist doctors chambers, there were no patients from this group at the headache clinic.
There were some limitations in this study. Firstly, the study sample though consisted only of school going children, no school was visited but rather, the data was collected from hospital records of patients who were students. Strict adherence to those particular records of students was done to minimize the error in data gathering. Though the specialized outpatient Headache Clinic is regarded as one of the highest centres for referral for headache patients, it does not reflect the disease burden within the community. Secondly, though the patients were evaluated by different neurologists at the specialized Headache Clinic, the observers’ bias was minimized by strictly following the IHS criteria (ICHD-II 2004) for diagnosis and classification of headache disorder. Thirdly, due to the retrograde nature of the study, some other aspects of headache in this group of patients (e.g. the child’s behavior, home and school environment, number of school days lost due to headache, attitude of parents and teachers to student’s headache and family history of migraine) were not evaluated. Finally, there is higher chance of recall error in children when asked about the frequency and character of the headaches within the last month or year. Because of the subjective nature of pain, self report measure is considered as the gold standard for pain assessment.30 Luckily enough, the specialized Headache Clinic in our setting also evaluated and cross checked the history of headache from accompanied persons of the children.
Conclusion
Headache is not simply a complaint but also a major health issue in children. This study aimed to highlight the characteristics of headache in young students who often seek medical advice for their problems. The higher frequency of headaches found among girls makes them more vulnerable. Sometimes headaches among girls are inappropriately treated or ignored. What has been discussed here so far is just an observation. There are many questions yet to be answered. Further studies should be conducted in every school, most importantly in rural areas and in girls’ school to determine the prevalence, underlying cause and the measures to be taken to prevent headache among school children in Bangladesh, a country where data recording and maintenance is scarce even for headaches in adults. This study will shed some light into the pattern of headache in school children.
Acknowledgements
The authors reported no conflict of interest and no funding was received in this work.
References
1. WHO report on South East Asia. Some facts and figures in Epilepsy. Avaialable at: http://www.searo.who.int/LinkFiles/Information_and_Documents_facts.
2. Oelkers-Ax R, Resch F. Headache in children: also a problem for child and adolescent psychiatry? Pathogenesis, comorbidity, therapy. Z Kinder Jugendpsychiatr Psychother 2002 Nov;30(4):281-293.
3. Carlsson J. Prevalence of headache in schoolchildren: relation to family and school factors. Acta Paediatr 1996 Jun;85(6):692-696.
4. Stovner LJ, Andree C. Prevalence of headache in Europe: a review for the Eurolight project. J Headache Pain 2010 Aug;11(4):289-299.
5. Bille BS. Migraine in school children. A study of the incidence and short-term prognosis, and a clinical, psychological and electroencephalographic comparison between children with migraine and matched controls. Acta Paediatr Suppl 1962 May;136(suppl):1-151.
6. Powers S, Patton S, Hommel KA, Hershey AD. Quality of life in childhood migraine: clinical impact and comparison to other chronic illnesses. Pediatrics 2003;112:1-5.
7. Bille BS. Migraine in school children. A study of the incidence and short-term prognosis, and a clinical, psychological and electroencephalographic comparison between children with migraine and matched controls. Acta Paediatr Suppl 1962 May;136:1-151.
8. Sillanpää M. Prevalence of headache in prepuberty. Headache 1983 Jan;23(1):10-14.
9. Linet MS, Stewart WF, Celentano DD, Ziegler D, Sprecher M. An epidemiologic study of headache among adolescents and young adults. JAMA 1989 Apr;261(15):2211-2216.
10. Stewart WF, Linet MS, Celentano DD, Van Natta M, Ziegler D. Age- and sex-specific incidence rates of migraine with and without visual aura. Am J Epidemiol 1991 Nov;134(10):1111-1120.
11. Sillanpää M. Changes in the prevalence of migraine and other headaches during the first seven school years. Headache 1983 Jan;23(1):15-19.
12. Rasmussen BK, Jensen R, Schroll M, Olesen J. Epidemiology of headache in a general population–a prevalence study. J Clin Epidemiol 1991;44(11):1147-1157.
13. Rasmussen BK, Olesen J. Migraine with aura and migraine without aura: an epidemiological study. Cephalalgia 1992 Aug;12(4):221-228, discussion 186.
14. Egermark-Eriksson I. Prevalence of headache in Swedish schoolchildren. A questionnaire survey. Acta Paediatr Scand 1982 Jan;71(1):135-140.
15. Hockaday JM. Migraine in children. J Maternal Childhealth 1991;16:146-147.
16. Abu-Arefe I, Russell G. Prevalence of headache and migraine in school children. BMJ 1994;308:765-769 .
17. Stewart WF, Lipton RB, Celentano DD, Reed ML. Prevalence of migraine headache in the United States. Relation to age, income, race, and other sociodemographic factors. JAMA 1992 Jan;267(1):64-69.
18. King NJ, Sharpley CF. Headache activity in children and adolescents. J Paediatr Child Health 1990 Feb;26(1):50-54.
19. Passchier J, Orlebeke JK. Headache and stress in school children: an epidemiological study. Cephalgia 1985;5:167-176 .
20. Saraceni G, Armani S, Botazzo S, Gesmundo E. Prevalence of migraine in 901 Venetian school children between 6 and 13 years. In: Lanzi G, Balottin U, Cernibori A, editors. Headache in children and adolescents. New York: Elsevier, 1989:181-89.
21. Anttila P, Metsahonkala L, Sillanpaa M. Long-term Trends in the Incidence of Headache in Finnish Schoolchildren. Pediatrics 2006;117:1197-1201.
22. Lateef TM, Merikangas KR, He J, Kalaydjian A, Khoromi S, Knight E, et al. Headache in a national sample of American children: prevalence and comorbidity. J Child Neurol 2009 May;24(5):536-543.
23. Kowal A, Pritchard D. Psychological characteristics of children who suffer from headache: a research note. J Child Psychol Psychiatry 1990 May;31(4):637-649.
24. Siddiqui SJ, Shamim SM, Hashmi AM. Prevalence and patterns of headache in school children in Karachi. J Pak Med Assoc 2006 May;56(5):215-217.
25. Bandell-Hoekstra IE, Abu-Saad HH, Passchier J, Frederiks CM, Feron FJ, Knipschild P. Prevalence and characteristics of headache in Dutch schoolchildren. Eur J Pain 2001;5(2):145-153.
26. Launer LJ, Terwindt GM, Ferrari MD. The prevalence and characteristics of migraine in a population-based cohort: the GEM study. Neurology 1999 Aug;53(3):537-542.
27. Molgaard CA, Rothrock J, Stang PE, Golbeck AL. Prevalence of migraine among Mexican Americans in San Diego, California: survey 1. Headache 2002 Oct;42(9):878-882.
28. Lipton RB, Stewart WF, Diamond S, Diamond ML, Reed M. Prevalence and burden of migraine in the United States: data from the American Migraine Study II. Headache 2001 Jul-Aug;41(7):646-657.
29. Zivadinov R, Willheim K, Jurjevic A, Sepic-Grahovac D, Bucuk M, Zorzon M. Prevalence of migraine in Croatia: a population-based survey. Headache 2001 Sep;41(8):805-812.
30. Merskey H, ed. Classification of chronic pain: descriptions of chronic pain syndromes and pain terms. Pain 1986;(suppl. 3):217.
|