|
Abstract
This is a case of Milk-AlKali syndrome in a patient who presented with the classical triad of hypercalcemia, metabolic alkalosis and renal impairment. The source of calcium was over-the-counter-calcium-containing antacid (Tums®). Milk-alkali syndrome was first recognized secondary to treatment of peptic ulcer disease with milk and absorbable alkali. Its incidence fell after the introduction of H2-blocker and proton pump inhibitor. However, it is one of the leading causes of hypercalcemia now adays because of the wide availability, increased marketing and use of calcium carbonate especially in osteoporosis prevention and treatment. The demographics of milk-alkali syndrome have changed compared to when it was initially described. The presentation could be acute, subacute or chronic. Early diagnosis, discounting calcium supplement and intravenous hydration are the mainstay of MAS management.
Keywords: Milk-alkali syndrome; MAS; Calcium-alkali syndrome; Hypercalcemia.
Introduction
Milk-alkali syndrome (MAS) was common when milk and absorbable alkali were the main treatment for peptic ulcer disease. The syndrome became rarer after the introduction of modern treatment for peptic ulcer disease such as H2-blocker. However, there has been a resurgence of MAS and now it is the third leading cause of hypercalcemia after primary hyperparathyroidism and malignancy. Here is a report of a case of MAS in a patient who took excess calcium carbonate as a treatment for heartburn. He was treated with intravenous saline and diuretic and had a full recovery.
Case Report
A 70-year-old male presented to the emergency department with multiple episodes of hematemisis over 24 hours and 6 days history of increasing heartburn, epigastric pain, headache, and malaise. He had been taking 15 to 25 Tums, which is a calcium carbonate antacid for heartburn, and that was equivalent to 7.5 to 15 g of elemental calcium. The patient was known to have gastroesophageal reflux disease (GERD), hypothyroid of post radioactive iodine treatment, and ischemic heart disease. On examination, he was found to be mildly confused and had dry oral mucosa with vital signs being within normal range.
Initial blood tests showed urea of 14.4 mmol/L, serum creatinine of 398 µmol/L, serum bicarbonate of 32 mmol/L, and serum calcium of 4.38 mmol/L. He was also found to have metabolic alkalosis. The patient was suspected to have milk alkali syndrome (MAS) and treated accordingly. Other investigations showed a low parathyroid hormone (PTH), normal thyroid test, normal serum protein electrophoresis (SPEP), no evidence of multiple myeloma in bone survey, and normal ultrasound of his kidneys.
Gastroenterology and nephrology services were consulted. The patient was treated with aggressive hydration and furosemide for 2 days. He also received 3 doses of calcitonin 300 IU. The patient was started on proton pump inhibitor and had upper endoscopy which showed severe esophagitis, (Fig. 1). All symptoms and laboratory tests gradually improved. Milk alkali syndrome was diagnosed based on clinical picture and laboratory findings.
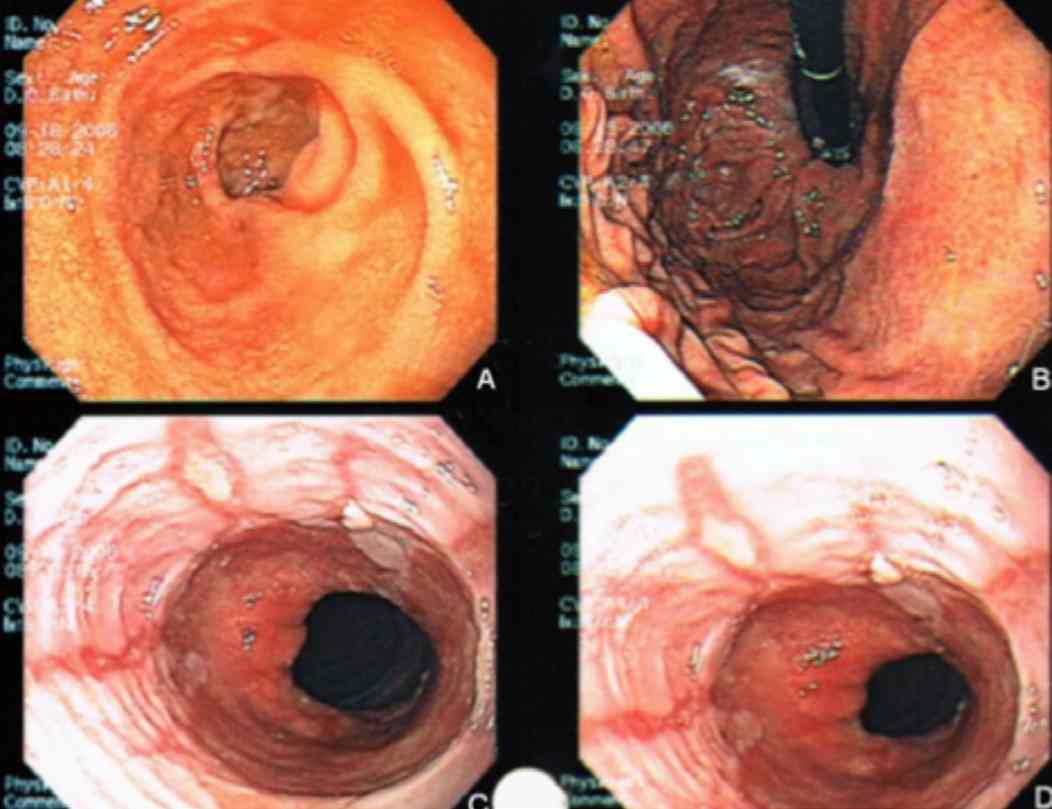
Figure 1: Pictures of the upper endoscopy showing: A & B) Normal looking duodenal and gastric mucosa respectively; C & D) Multiple circumferential mucosal breaks corresponding to Los Angeles grade D esophagitis.
Discussion
Milk alkali syndrome (MAS) consists of a triad of hypercalcemia, metabolic alkalosis and variable degrees of renal insufficiency as a result of ingestion of large amounts of calcium and absorbable alkali.1 The classical MAS was more commonly seen when milk and absorbable alkali (Sippy’s regimen) were the main treatment of peptic ulcer disease.2,3 Some patients on Sippy’s regimen developed renal failure and metabolic alkalosis as reported by Hardt and Rivers in 1923.4 However, it was not until 1936 when Cope described hypercalcemia for the first time as an element of milk-alkali syndrome.5
The syndrome incidence fell after the introduction of modern treatments for peptic ulcer disease such as H2-blockers in 1970s and proton pump inhibitors later on. The syndrome accounted for less than 2% of cases admitted with hypercalcemia before 1990; but after 1990, there has been a resurgence of the syndrome. MAS was found in two studies to be third behind hyperparathyroidism and malignancy as a cause of hypercalcemia requiring hospitalization, with incidence ranging between 8.8% and 12%.2,6 The source of calcium in the modern version of MAS is calcium carbonate given for several indications like, osteoporosis treatment and prevention, as a phosphate binder in renal failure, with prolonged corticosteroid therapy and as over the counter antacid. In East Asia, chewing betel nuts is a popular cultural activity, and it is mixed with oyster shell paste containing calcium carbonate to neutralize the bitter taste of the betel nuts. This has been reported to be a cause of MAS in many reports.7-9
The modern form of MAS differs from the classical one in many aspects. The demographics of MAS changed from being middle-aged male dominated to female-dominated with average age of 50 years.2 Over-the-counter calcium carbonate is the main source of calcium and alkali in the modern MAS. Hyperphosphatemia is rare nowadays and this has been contributed to the less prevalent consumption of large quantities of phosphorus rich dairy products and the phosphate-binding properties of calcium carbonate.1
The diagnosis of MAS depends on the history of excessive calcium and alkali ingestion, the finding of hypercalcemia, variable degree of renal impairment and the exclusion of other causes. The pathophysiology of MAS is complex. While increased calcium intake is the trigger, the reduction in renal excretion of calcium is the main abnormality. This is secondary to reduction in glomerular filtration rate (GFR) and increase in tubular reabsorption of calcium due to alkalosis. Hypercalcemia reduces GFR directly by inducing renal vasoconstriction and indirectly by reducing extracellular volume.1,10,11
Three forms of MAS have been reported, acute, subacute, and chronic.1,5 Nausea, vomiting, headache, dizziness, irritability and confusion are some of early signs and symptoms. Myalgia, tremor, polyuria, polydipsia, nephrocalcinosis, and ectopic calcification are typically found in chronic phase of MAS. Examples of ectopic calcification include ocular, liver, adrenal, bone, lungs, periarticular tissue, and subcutaneous tissue calcification.1 The first and most essential part of managing MAS is early diagnosis and discontinuing the calcium containing alkali. Intravenous hydration with isotonic saline to induce diuresis is the treatment of choice. Furosemide can be added once intracellular volume has been restored. Pamidronate has been used to treat MAS; however, it was associated with hypocalcemia in some patients.2,12 This might be attributed to the late onset of action which is around 24 hours. Hemodialysis should be considered in refractory hypercalcemia and severe renal impairment.
Conclusion
To the best of our knowledge, this is the first paper reporting and discussing milk alkali syndrome in Oman Medical Journal. We would like to raise the attention to this syndrome since it is a major cause of hypercalcemia in the last 20 years and it might result in major complications. Missing the diagnosis may result in unnecessary surgeries as reported by Beall and Scofield when 10% of the patients with MAS underwent unnecessary parathyroid exploration.6 It may also result in permanent renal function impairment.10 We also would like to join other authors13,14 who suggested renaming the syndrome to calcium-alkali syndrome (CAS) rather than MAS or modern MAS since calcium carbonate is the main source of calcium.2,10
Acknowledgements
The authors reported no conflict of interest and no funding was received in this work.
References
1. Medarov BI. Milk-alkali syndrome. Mayo Clin Proc 2009 Mar;84(3):261-267.
2. Scofield R, Pourmotabbed P, Khardori R. Milk-Alkali Syndrome, (Accessed August 1, 2011, at http://emedicine.medscape.com/article/123324-overview)
3. Sippy BW. Landmark article May 15, 1915: Gastric and duodenal ulcer. Medical cure by an efficient removal of gastric juice corrosion. By Bertram W. Sippy. JAMA 1983 Oct;250(16):2192-2197.
4. Hardt L, Rivers A. Toxic manifestations following the alkaline treatment of peptic ulcer. Arch Intern Med 1923;31:171-180 .
5. Cope CL. Base changes in the alkalosis produced by the treatment of gastric ulcer with alkalies. Clin Sci 1936;2:287-300.
6. Beall DP, Scofield RH. Milk-alkali syndrome associated with calcium carbonate consumption. Report of 7 patients with parathyroid hormone levels and an estimate of prevalence among patients hospitalized with hypercalcemia. Medicine (Baltimore) 1995 Mar;74(2):89-96.
7. Wu K-D, Chuang R-B, Wu F, Hsu W-A, Jan I-S, Tsai K-S. The milk-alkali syndrome caused by betel nuts in oyster shell paste. Clin Toxicol 1996;34:741-745 .
8. Lin SH, Lin YF, Cheema-Dhadli S, Davids MR, Halperin ML. Hypercalcaemia and metabolic alkalosis with betel nut chewing: emphasis on its integrative pathophysiology. Nephrol Dial Transplant 2002 May;17(5):708-714.
9. Yiang G, Hsu B, Horng-Jyh H, et al. Betel nut induced milk-alkali syndrome. Tzu Chi Med J 2005;17:265-268.
10. Beall DP, Henslee HB, Webb HR, Scofield RH. Milk-alkali syndrome: a historical review and description of the modern version of the syndrome. Am J Med Sci 2006 May;331(5):233-242.
11. McGuinness B, Logan JI. Milk alkali syndrome. Ulster Med J 2002 Nov;71(2):132-135.
12. Picolos MK, Lavis VR, Orlander PR. Milk-alkali syndrome is a major cause of hypercalcaemia among non-end-stage renal disease (non-ESRD) inpatients. Clin Endocrinol (Oxf) 2005 Nov;63(5):566-576.
13. Kaklamanos M, Perros P. Milk alkali syndrome without the milk. BMJ 2007 Aug;335(7616):397-398.
14. Patel AM, Goldfarb S. Got calcium? Welcome to the calcium-alkali syndrome. J Am Soc Nephrol 2010 Sep;21(9):1440-1443.
|