The eye is a unique anatomical organ, protected by the continuous flow of tears having antimicrobial compounds. However, it is often colonized by a range of microorganisms.1 Eye infections can be caused by several microorganisms, such as bacteria, viruses, parasites, or fungi, and they are able to develop a spectrum of diseases and symptoms. The symptoms of infections are variable, depending on the type of infection and causative agents.2 Ocular infections comprise keratitis, endophthalmitis, conjunctivitis, blepharitis, stye, orbital cellulitis, and dacryocystitis manifestations.3 Infectious keratitis is an infection of the cornea that might be associated with ocular surgery, trauma, contact lens use, suppression of the immune system (such as diabetes), chronic use of topical steroids, or immunomodulatory therapies. Bacterial infection is the most common cause of infectious keratitis.4 Endophthalmitis is a potentially blinding intraocular infection and inflammation, resulting from the entry of bacteria into the interior part of the eye.5 Other inflammatory diseases of the eye usually occur through bacterial infection.6–8 The most common causative bacteria are Staphylococcus aureus, coagulase-negative staphylococci, viridans group streptococci, and Pseudomonas aeruginosa.9,10
Understanding the epidemiology of eye infections in a region is essential to reinforce effective prevention and control strategies. There is no comprehensive data regarding bacterial ocular infections in Iran. Therefore, the aim of this study was to assess the prevalence of frequent bacteria that cause ocular infections during 21 years in Iran using a systematic review and meta-analysis.
Methods
In the present systematic review and meta-analysis study, all procedures for identification of papers were carried out in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. This study was approved by the Ethics Committee of Shahrekord University of Medical Sciences (Register code: IR.SKUMS.REC.1400.091).
We conducted a systematic search of studies published by Iranian authors from January 2000 to December 2020 in Web of Science, PubMed, Scopus, and Embase. Records were managed by EndNote X9.0 software to exclude duplicates. We used eye infection-related key terms (conjunctivitis, keratitis, stye, uveitis, endophthalmitis, eye disorder, ocular infection, and eye infection) and key terms to identify Iran. To identify the missing studies, we also searched bibliographies of retrieved articles for additional references.
Cross-sectional or cohort studies that reported the prevalence of S. aureus, S. epidermidis, viridans streptococci, or P. aeruginosa in eye infections were considered. The titles, abstracts, and full texts were screened independently by two reviewers to determine the articles that met the inclusion criteria, and any discrepancies were resolved with a third investigator or by consensus. Articles published in the English or Persian language that were indexed in PubMed or Scopus with the following characteristics and reported the prevalence of S. aureus, S. epidermidis, viridans streptococci, or P. aeruginosa in eye infections were included. Additionally, studies conducted by non-Iranian authors on the Iranian population or samples were also assessed. The studies without reports of bacterial prevalence in eye infections were excluded. The studies with insufficient, unclear, or missing information were also excluded from the meta-analysis. We also excluded studies with a sample size < 10 isolates, non-human studies, published studies in languages other than English or Persian, review articles, meta-analyses or systematic reviews, and congress abstracts.
Data collection was performed in parallel by two investigators who performed the literature searches. Variables such as the first author’s name, the time the study was performed, publication date, the study setting, site of infection, sample size (number of bacterial isolates obtained from eye infections), and the prevalence of the mentioned bacteria were extracted.
Analysis of data was performed using Comprehensive. Meta-Analysis software version 2.2 (Bio-stat Company). Meta-analysis was performed using random effects model to estimate the pooled prevalence and corresponding 95% CI. Statistical heterogeneity between and within groups was estimated by the Q statistic and I2 index. The funnel plots, Duval and Tweedie trim, and fill methods were carried out to evaluate the evidence of publication bias.
Results
A total of 345 articles were retrieved using the search strategy; 285 were excluded based on the index and review of the titles and abstracts, leaving 60 articles for full-text review. Full-text screening excluded 33 studies, resulting in 27 eligible studies. Figure 1 shows the study selection process and reasons for exclusion. The main characteristics of the included studies and the prevalence of S. aureus, S. epidermidis, viridans streptococci, and P. aeruginosa in eye infections are shown in Table 1.
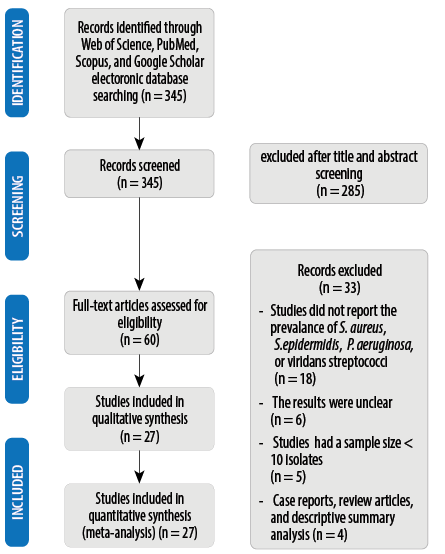 Figure 1: Summary of the literature search and study selection.
Figure 1: Summary of the literature search and study selection.
Table 1: Characteristics of studies included in the meta-analysis.
|
Tabatabaei et al,11
|
2020
|
2008–2018
|
Tehran
|
Iritis and/or vitritis
|
27.1
|
-
|
2.8
|
4.9
|
|
Soleimani et al,12
|
2020
|
2008–2017
|
Tehran
|
Keratitis
|
4.3
|
10.8
|
1.1
|
10.8
|
|
Abtahi et al,13
|
2020
|
2016–2019
|
Shiraz
|
Orbital cellulitis
|
2
|
2
|
-
|
-
|
|
Feizi et al,14
|
2019
|
2017
|
Tehran
|
Persistent corneal epithelial defects
|
2
|
17.5
|
2
|
-
|
|
Zare et al,15
|
2019
|
2017–2018
|
Tehran
|
Corneal ulcers
|
6
|
-
|
1
|
3
|
|
Nemati et al,16
|
2018
|
2014–2015
|
Guilan
|
Nasolacrimal duct obstruction
|
4.1
|
16.6
|
-
|
11.1
|
|
Owji et al,17
|
2018
|
Unknown
|
Shiraz
|
Nasolacrimal duct obstruction
|
18
|
62.6
|
6
|
-
|
|
Eghtedari et al,18
|
2018
|
Unknown
|
Shiraz
|
Corneal ulcer
|
7.9
|
6.3
|
-
|
9.5
|
|
Heidari et al,19
|
2018
|
2016–2017
|
Shiraz
|
Corneal infection
|
7.1
|
-
|
-
|
12.5
|
|
Faridi et al,20
|
2018
|
2016
|
Tehran
|
External ocular infection
|
9.8
|
-
|
-
|
-
|
|
Eshraghi et al,21
|
2016
|
Unknown
|
Tehran
|
Unilateral nasolacrimal duct obstruction
|
7
|
40.8
|
11.2
|
-
|
|
Faghri et al,22
|
2016
|
2013
|
Isfahan
|
Severe pain and corneal ulcers
|
2.5
|
49.3
|
-
|
6.4
|
|
Rahimi et al,23
|
2015
|
2008–2012
|
Tehran
|
Bacterial keratitis
|
3.8
|
6.1
|
6.6
|
24.7
|
|
Abrishami et al,24
|
2015
|
Unknown
|
Mashhad
|
Postoperative endophthalmitis
|
9.3
|
9.3
|
-
|
6.2
|
|
Oryan et al,25
|
2014
|
2012–2013
|
Isfahan
|
Keratitis infections
|
2.6
|
49.3
|
-
|
6.5
|
|
Sharifi et al,26
|
2013
|
2007–2010
|
Yasuj
|
Ocular trauma
|
2.8
|
3.8
|
1
|
1
|
|
Eshraghi etl al,27
|
2013
|
2007–2010
|
Tehran
|
Acute dacryocystitis, lacrimal sac empyema underwent incision, and drainage
|
25
|
-
|
12.5
|
-
|
|
Ghasemi et al,28
|
2013
|
Unknown
|
Tehran
|
Serious sulfur mustard-induced ocular injuries
|
3.5
|
7
|
0.7
|
-
|
|
Falavarjani et al,29
|
2012
|
2006–2011
|
Tehran
|
Endophthalmitis
|
15.3
|
24.6
|
1.5
|
23
|
|
Rahimi et al,30
|
2012
|
2005–2009
|
Shiraz
|
Acute endophthalmitis
|
17.1
|
5.7
|
-
|
5.7
|
|
Bagheri et al,31
|
2012
|
1997–2007
|
Tehran
|
Orbital and preseptal cellulitis
|
7.5
|
-
|
-
|
-
|
|
Hosseini et al,32
|
2012
|
2008
|
Shiraz
|
Endophthalmitis
|
11.3
|
31.8
|
18.1
|
2.2
|
|
Karimian et al,33
|
2011
|
Unknown
|
Tehran
|
Chronic blepharitis
|
3
|
57
|
-
|
-
|
|
Sedghipour et al,34
|
2011
|
2000–2003
|
Tabriz
|
Corneal ulcer
|
-
|
23.2
|
-
|
-
|
|
Razavi et al,35
|
2010
|
2007–2008
|
Mashhad
|
Acute and chronic dacryocystitis
|
13.1
|
47.5
|
1.6
|
3.2
|
|
Khosravi et al,36
|
2007
|
2005–2006
|
Ahwaz
|
Ocular infection
|
2.8
|
7.2
|
1.5
|
5.3
|
In 26 studies, the prevalence of S. aureus in eye infections was investigated. The pooled prevalence for S. aureus isolates was 6.7% (95% CI: 4.6–9.6; range = 0.5–27.1%) [Figure 2]. There was a significant heterogeneity among the 26 studies (χ2 = 136.101; p < 0.001; I2 = 81.6%). The symmetric funnel plot showed no evidence of publication bias [Supplement 1a]. Furthermore, using Duval and Tweedie’s trim and fill procedures, no evidence of publication bias was found for any of the measures.
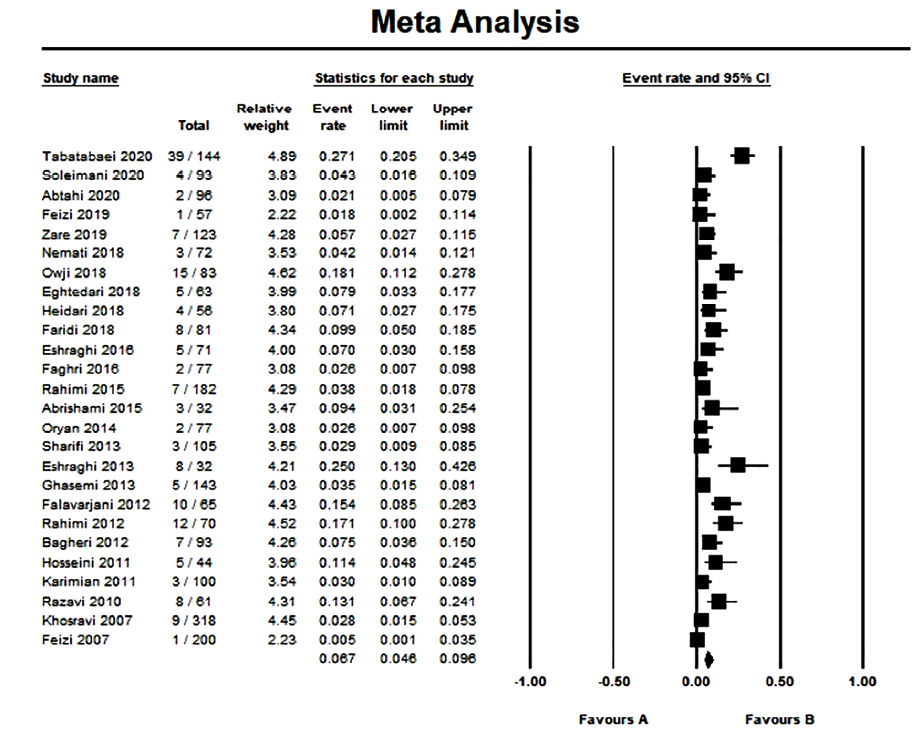 Figure 2: Forest plot of prevalence of ocular infections causative S. aureus isolates in Iran.
Figure 2: Forest plot of prevalence of ocular infections causative S. aureus isolates in Iran.
According to the included studies, the frequency of S. epidermidis isolates was investigated in 21 studies. The pooled prevalence of S. epidermidis isolates was estimated at 19.1% (95% CI: 12.5–28.1; range = 2.1–62.7%) [Figure 3]. There was a significant heterogeneity among the 21 studies (χ2 = 328.470; p < 0.001; I2 = 93.9%). There was no evidence of publication bias [Supplement 1b].
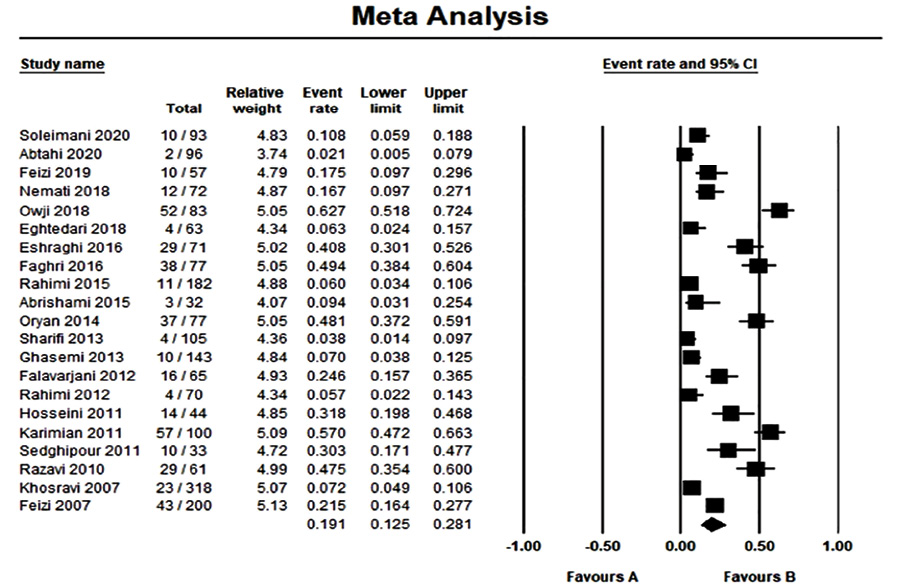 Figure 3: Forest plot of prevalence of ocular infections causative S. epidermidis isolates in Iran.
Figure 3: Forest plot of prevalence of ocular infections causative S. epidermidis isolates in Iran.
In 15 studies on viridans group streptococci, the pooled prevalence was 3.3% (95% CI: 1.8–5.8; range = 0.7%–18.2%) [Figure 4]. There was a significant heterogeneity among the 15 studies (χ2 = 54.2; p < 0.001; I2 = 74.2%). Publication bias was assessed by funnel plot for the standard error by logit event, with no evidence of bias [Supplement 1c]. Additionally, Duval and Tweedie’s trim and fill tests suggested that there was no notable evidence of publication bias.
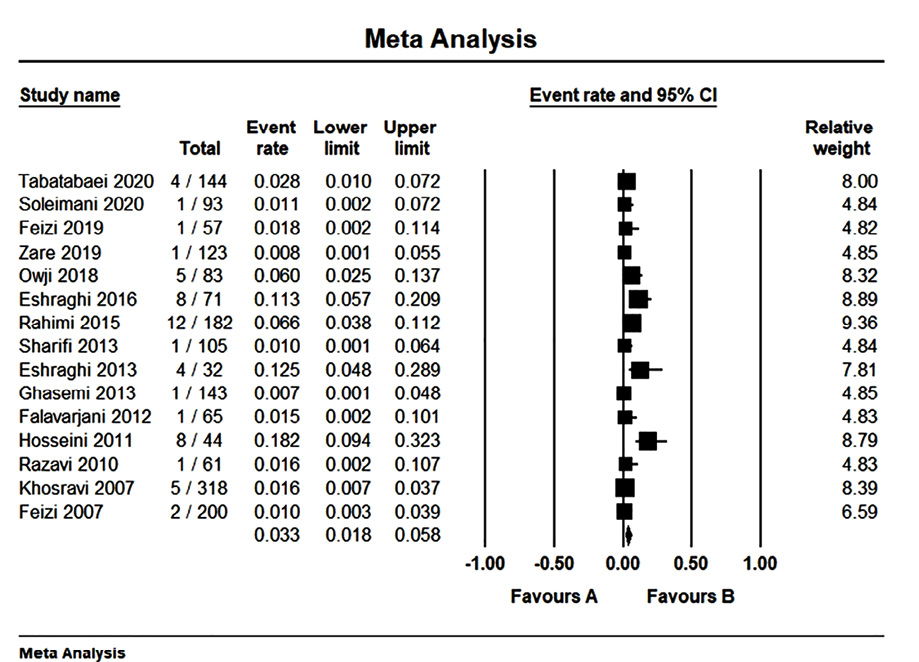 Figure 4: Forest plot of prevalence of ocular infections causative viridans streptococci in Iran.
Figure 4: Forest plot of prevalence of ocular infections causative viridans streptococci in Iran.
We found 17 articles that investigated the prevalence of P. aeruginosa in bacterial eye infections. The pooled prevalence of P. aeruginosa isolates was estimated at 6.9% (95% CI: 4.4–10.6; range = 0.5–24.7%) [Figure 5]. Based on the Q-statistic and I2 index, heterogeneity was significant (χ2 = 91.699; p < 0.001; I2 = 82.6%). Also, there was no evidence of publication bias [Supplement 1d].
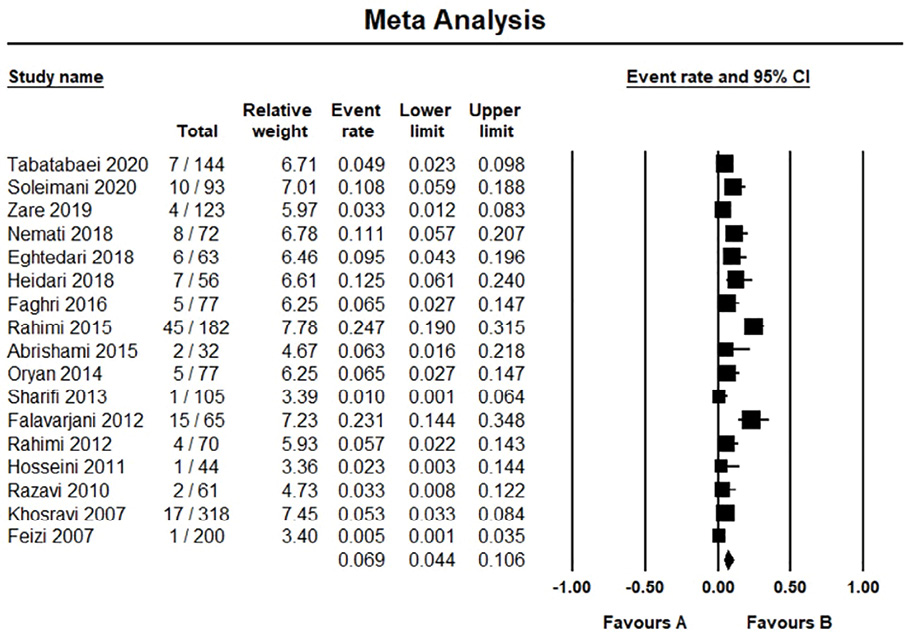 Figure 5: Forest plot of prevalence of ocular infections causative P. aeruginosa isolates in Iran.
Figure 5: Forest plot of prevalence of ocular infections causative P. aeruginosa isolates in Iran.
Discussion
Bacteria are the major contributors to ophthalmic diseases worldwide. The dominant causative bacterial agents of ocular infections are staphylococci, streptococci, and P. aeruginosa.9,10,38 To the best of our knowledge, this study is the first systematic review on the prevalence of S. aureus, S. epidermidis, P. aeruginosa, and viridans group streptococci isolates that caused eye infections in Iran. According to the meta-analysis results, the pooled prevalence of S. aureus isolates that caused these infections was 6.7%. In a previous systematic review conducted on bacterial profile of ocular infections in several developed and developing countries (including Nigeria, India, Ethiopia, Japan, USA, and Malaysia), the average prevalence of S. aureus was more than 20%.38 Furthermore, our analysis indicated that the pooled prevalence of S. epidermidis isolates was 19.1%, and it was the most common agent responsible for eye infections. Various prevalence rates of S. epidermidis or coagulase-negative staphylococci were reported in previous studies.38–46 These discrepancies may be related to the type of eye-associated infections. Besides, a variety of factors, such as contact lens wearing, immune system status, anatomical disruption, and traumatic inoculation of the organisms by foreign bodies, could determine the prevalence and distribution of the type of bacterial agents associated with ocular infections. These factors may lead to infection development by normal flora such as members of the staphylococci.38 S. epidermidis is the most commonly found bacteria, colonizing the mucosa and lid margins. Also, underlying diseases (such as diabetes) may affect the S. aureus colonization in the eyes and its subsequent prevalence in such infections. Geographical climate (heat and humidity) has been reported as another factor that affects the composition of ocular surface flora.47
Our analysis indicated that the pooled prevalence of viridans streptococci isolates was 3.3%. In a retrospective study in the USA, the viridans streptococci were responsible for the majority of endophthalmitis caused by Streptococcus species (71%).48 Another retrospective study from the USA indicated that 11% of ocular infections and 12.1% of endophthalmitis cases were related to viridans group streptococci.46,49 The prevalence of these bacteria was 2.8% in community-acquired bacterial ocular infections in India.40 Various rates of viridans group streptococci associated with ocular infections were reported from several regions, such as Spain (5%),50 Mexico (14.3%),51 Nigeria (1.5%),38 and the UK (0.4%).52 This diversity may be related to different types of ocular infections.
The pooled prevalence of P. aeruginosa isolates was estimated at 6.9%. Greater rates were reported from Taiwan (35.2%),43 Ethiopia (11.7%),44 India (10.7%,53 21%,38 and 44%54), Nigeria (10.1%), Japan (9.7%), Malaysia (16%),38 and the USA (8–16%).38,46 An analysis in the UK showed that the prevalence of P. aeruginosa was 7.2%.45 However, lower frequencies were reported from India (3%) and Ethiopia (4.9%).38 P. aeruginosa utilizes various virulence factors and mechanisms, such as exotoxins, proteases, elastases, and biofilm formation to develop an infection in the eye tissues. It is a common causative agent in cases of ocular infections, especially corneal ulcer infection and keratitis associated with contact lens use. Moreover, the current evidence suggests that the majority of such infections are related to P. aeruginosa genotypes that encode the exotoxin U. Constant exposure to a sub-inhibitory concentration of lens cleaning solutions and biocides can contribute to resistance to disinfectants. The prevalence of infection caused by P. aeruginosa also depends on other predisposing factors, such as ocular surgery, immunodeficiency, diabetes mellitus, and rheumatoid arthritis. These situations may lead to severe infections such as endophthalmitis.38,55–58
Conclusion
S. epidermidis was the most common bacterial agent responsible for ocular infections in Iran (19.1%). The prevalence of P. aeruginosa isolates was 6.9%, and S. aureus and viridans group streptococci accounted for 6.7% and 3.3% of eye-associated infections. Our results will contribute to understanding bacterial agent contributions in ocular infections in Iran.
Disclosure
The authors declared no conflicts of interest. No funding was received for this study. This study was supported by Shahrekord University of Medial Sciences (Project no: 3623).
references
- 1. McDermott AM. Antimicrobial compounds in tears. Exp Eye Res 2013 Dec;117:53-61.
- 2. Sharma S. Diagnosis of infectious diseases of the eye. Eye (Lond) 2012 Feb;26(2):177-184.
- 3. O’Callaghan RJ. The pathogenesis of Staphylococcus aureus eye infections. Pathogens 2018 Jan;7(1):9.
- 4. Al-Mujaini A, Al-Kharusi N, Thakral A, Wali UK. Bacterial keratitis: perspective on epidemiology, clinico-pathogenesis, diagnosis and treatment. Sultan Qaboos Univ Med J 2009 Aug;9(2):184-195.
- 5. Novosad BD, Callegan MC. Severe bacterial endophthalmitis: towards improving clinical outcomes. Expert Rev Ophthalmol 2010 Oct;5(5):689-698.
- 6. Lindsley K, Nichols JJ, Dickersin K. Interventions for acute internal hordeolum. Cochrane Database Syst Rev 2013 Apr;4(4):CD007742.
- 7. Danishyar A, Sergent SR. Orbital cellulitis. StatPearls; 2020.
- 8. Bharathi MJ, Ramakrishnan R, Maneksha V, Shivakumar C, Nithya V, Mittal S. Comparative bacteriology of acute and chronic dacryocystitis. Eye (Lond) 2008 Jul;22(7):953-960.
- 9. Watson S, Cabrera-Aguas M, Khoo P. Common eye infections. Aust Prescr 2018 Jun;41(3):67-72.
- 10. Getahun E, Gelaw B, Assefa A, Assefa Y, Amsalu A. Bacterial pathogens associated with external ocular infections alongside eminent proportion of multidrug resistant isolates at the University of Gondar Hospital, northwest Ethiopia. BMC Ophthalmol 2017 Aug;17(1):151.
- 11. Tabatabaei SA, Soleimani M, Mirshahi R, Bohrani B, Aminizade M. Culture-proven endogenous endophthalmitis: microbiological and clinical survey. Int Ophthalmol 2020 Dec;40(12):3521-3528.
- 12. Soleimani M, Tabatabaei SA, Mohammadi SS, Valipour N, Mirzaei A. A ten-year report of microbial keratitis in pediatric population under five years in a tertiary eye center. J Ophthalmic Inflamm Infect 2020 Nov;10(1):35.
- 13. Abtahi SM, Eghtedari M, Hosseini S, Shirvani M, Talebi A, Masihpoor N, et al. Non-medial infectious orbital cellulitis: etiology, causative organisms, radiologic findings, management and complications. J Ophthalmic Inflamm Infect 2020 Sep;10(1):22.
- 14. Feizi S, Masoudi A, Hosseini SB, Kanavi MR, Javadi MA. Microbiological evaluation of bandage soft contact lenses used in management of persistent corneal epithelial defects. Cornea 2019 Feb;38(2):146-150.
- 15. Zare M, Torbati PM, Asadi-Amoli F, Talebnejad M, Parvizi M, Nasiri Z, et al. Microbiological profile of corneal ulcers at a tertiary referral center. Med Hypothesis Discov Innov Ophthalmol 2019;8(1):16-21.
- 16. Nemati S, Mojtahedi A, Montazeri S, Pahlavan PA. Microbial etiology and antibacterial resistance patterns of dacryocystorhinostomy cases in the north of Iran. Asian J Pharm Clin Res 2018;11(7):407-411.
- 17. Owji N, Zareifard A. Bacterial flora of the conjunctiva one year after dacryocystorhinostomy. Middle East Afr J Ophthalmol 2018 Jan-Mar;25(1):35-39.
- 18. Eghtedari M, Beigi V, Mostafavi E. Pediatric microbial keratitis: a tertiary care center report. Shiraz E Med J 2018;19(9):e66197.
- 19. Heidari H, Hadadi M, Sedigh Ebrahim-Saraie H, Mirzaei A, Taji A, Hosseini SR, et al. Characterization of virulence factors, antimicrobial resistance patterns and biofilm formation of Pseudomonas aeruginosa and Staphylococcus spp. strains isolated from corneal infection. J Fr Ophtalmol 2018 Nov;41(9):823-829.
- 20. Faridi A, Kareshk AT, Fatahi-Bafghi M, Ziasistani M, Ghahraman MR, Seyyed-Yousefi SZ, et al. Detection of methicillin-resistant Staphylococcus aureus (MRSA) in clinical samples of patients with external ocular infection. Iran J Microbiol 2018 Aug;10(4):215-219.
- 21. Eshraghi B, Alemzadeh SA, Abedinifar Z. Conjunctival bacterial flora in fellow eyes of patients with unilateral nasolacrimal duct obstruction and its changes after successful dacryocystorhinostomy surgery. J Curr Ophthalmol 2016 Dec;29(1):59-62.
- 22. Faghri J, Zandi A, Peiman A, Fazeli H, Esfahani BN, Safaei HG, et al. Study on prevalence, antibiotic susceptibility, and tuf gene sequence-based genotyping of species-level of coagulase-negative staphylococcus isolated from keratitis caused by using soft contact lenses. Eye Contact Lens 2016 Mar;42(2):115-119.
- 23. Rahimi F, Hashemian MN, Khosravi A, Moradi G, Bamdad S. Bacterial keratitis in a tertiary eye centre in Iran: a retrospective study. Middle East Afr J Ophthalmol 2015 Apr-Jun;22(2):238-244.
- 24. Abrishami M, Hashemi B, Abrishami M, Abnous K, Razavi-Azarkhiavi K, Behravan J. PCR detection and identification of bacterial contaminants in ocular samples from post-operative endophthalmitis. J Clin Diagn Res 2015 Apr;9(4):NC01-NC03.
- 25. Oryan G, Faghri J, Fazeli H, Zandi A, Hosseini N-S, Sedighi M, et al. A Study of the prevalence and antibacterial resistance of coagulase negative Staphylococci in keratitis infections following the use of soft contact lenses. Majallah-i Danishkadah-i Pizishki-i Isfahan 2014;32(277):273-281.
- 26. Sharifi B, Shirazi HR, Malek-Hosseini SH, Afzalian E. Evaluation of positive culture during the initial healing of penetrating ocular trauma. Life Sci J 2013;10(7s):539-544.
- 27. Eshraghi B, Hashemian H, Fard MA, Safizadeh M. Lacrimal sac empyema incision and drainage followed by early external dacryocystorhinostomy. Orbit 2013 Oct;32(5):278-280.
- 28. Ghasemi H, Owlia P, Ghazanfari T, Yaraee R, Saderi H, Soroush MR, et al. Conjunctival microbial florae in patients with seriously sulfur mustard induced eye injuries. Cutan Ocul Toxicol 2013 Mar;32(1):13-17.
- 29. Falavarjani KG, Nekoozadeh S, Modarres M, Parvaresh MM, Hashemi M, Soodi R, et al. Isolates and antibiotic resistance of culture-proven endophthalmitis cases presented to a referral center in Tehran. Middle East Afr J Ophthalmol 2012 Oct;19(4):361-363.
- 30. Rahimi M, Ghassemifar V, Nowroozzadeh MH. Outcome of endophthalmitis treatment in a tertiary referral center in southern Iran. Middle East Afr J Ophthalmol 2012 Jan;19(1):107-114.
- 31. Bagheri A, Tavakoli M, Aletaha M, Salour H, Ghaderpanah M. Orbital and preseptal cellulitis: a 10-year survey of hospitalized patients in a tertiary eye hospital in Iran. Int Ophthalmol 2012 Aug;32(4):361-367.
- 32. Hosseini H, Ashraf MJ, Saleh M, Nowroozzadeh MH, Nowroozizadeh B, Abtahi MB, et al. Effect of povidone-iodine concentration and exposure time on bacteria isolated from endophthalmitis cases. J Cataract Refract Surg 2012 Jan;38(1):92-96.
- 33. Karimian F, Zarei-Ghanavati S, A BR, Jadidi K, Lotfi-Kian A. Microbiological evaluation of chronic blepharitis among Iranian veterans exposed to mustard gas: a case-controlled study. Cornea 2011 Jun;30(6):620-623.
- 34. Sedghipour MR, Sorkhabi R, Shenasi A, Dehghan H. Outcome of penetrating keratoplasty in corneal ulcer: a single-center experience. Clin Ophthalmol 2011;5:1265-1268.
- 35. Razavi ME, Ansari-Astaneh MR, Farzadnia M, Rahmaniyan H, Moghiman T. Bacteriological evaluation of adult dacryocystitis in Iran. Orbit 2010 Oct;29(5):286-290.
- 36. Khosravi AD, Mehdinejad M, Heidari M. Bacteriological findings in patients with ocular infection and antibiotic susceptibility patterns of isolated pathogens. Singapore Med J 2007 Aug;48(8):741-743.
- 37. Feizi S, Jadidi K, Naderi M, Shahverdi S. Corneal interface contamination during laser in situ keratomileusis. J Cataract Refract Surg 2007 Oct;33(10):1734-1737.
- 38. Teweldemedhin M, Gebreyesus H, Atsbaha AH, Asgedom SW, Saravanan M. Bacterial profile of ocular infections: a systematic review. BMC Ophthalmol 2017 Nov;17(1):212.
- 39. Ramesh S, Ramakrishnan R, Bharathi MJ, Amuthan M, Viswanathan S. Prevalence of bacterial pathogens causing ocular infections in South India. Indian J Pathol Microbiol 2010 Apr-Jun;53(2):281-286.
- 40. Bharathi MJ, Ramakrishnan R, Shivakumar C, Meenakshi R, Lionalraj D. Etiology and antibacterial susceptibility pattern of community-acquired bacterial ocular infections in a tertiary eye care hospital in south India. Indian J Ophthalmol 2010 Nov-Dec;58(6):497-507.
- 41. Gao W, Xia T, Chen HB, Pan XJ, Huang YS, Wang X, et al. Ocular bacterial infections at a tertiary eye center in China: a 5-year review of pathogen distribution and antibiotic sensitivity. Int J Ophthalmol 2020 Jan;13(1):54-60.
- 42. Al-Dhaheri HS, Al-Tamimi MD, Khandekar RB, Khan M, Stone DU. Ocular pathogens and antibiotic sensitivity in bacterial keratitis isolates at King Khaled Eye Specialist Hospital, 2011 to 2014. Cornea 2016 Jun;35(6):789-794.
- 43. Liu HY, Chu HS, Wang IJ, Chen WL, Hu FR. Microbial keratitis in Taiwan: a 20-year update. Am J Ophthalmol 2019 Sep;205:74-81.
- 44. Teweldemedhin M, Saravanan M, Gebreyesus A, Gebreegziabiher D. Ocular bacterial infections at Quiha Ophthalmic Hospital, Northern Ethiopia: an evaluation according to the risk factors and the antimicrobial susceptibility of bacterial isolates. BMC Infect Dis 2017 Mar;17(1):207.
- 45. Tavassoli S, Nayar G, Darcy K, Grzeda M, Luck J, Williams OM, et al. An 11-year analysis of microbial keratitis in the South West of England using brain-heart infusion broth. Eye (Lond) 2019 Oct;33(10):1619-1625.
- 46. Geevarghese A, Shah P, Lopez J, Tsui E, Raju L. Common microbes and antibiotic resistance in ocular infections at an urban public tertiary care hospital. Ocul Immunol Inflamm 2022;30(2):481-486.
- 47. Grzybowski A, Brona P, Kim SJ. Microbial flora and resistance in ophthalmology: a review. Graefes Arch Clin Exp Ophthalmol 2017 May;255(5):851-862.
- 48. Kuriyan AE, Weiss KD, Flynn HW Jr, Smiddy WE, Berrocal AM, Albini TA, et al. Endophthalmitis caused by streptococcal species: clinical settings, microbiology, management, and outcomes. Am J Ophthalmol 2014 Apr;157(4):774-780.e1.
- 49. Gentile RC, Shukla S, Shah M, Ritterband DC, Engelbert M, Davis A, et al. Microbiological spectrum and antibiotic sensitivity in endophthalmitis: a 25-year review. Ophthalmology 2014 Aug;121(8):1634-1642.
- 50. de Paula A, Oliva G, Barraquer RI, de la Paz MF. Prevalence and antibiotic susceptibility of bacteria isolated in patients affected with blepharitis in a tertiary eye centre in Spain. Eur J Ophthalmol 2020 Sep;30(5):991-997.
- 51. Chirinos-Saldaña P, Bautista de Lucio VM, Hernandez-Camarena JC, Navas A, Ramirez-Miranda A, Vizuet-Garcia L, et al. Clinical and microbiological profile of infectious keratitis in children. BMC Ophthalmol 2013 Oct;13(1):54.
- 52. Orlans HO, Hornby SJ, Bowler IC. In vitro antibiotic susceptibility patterns of bacterial keratitis isolates in Oxford, UK: a 10-year review. Eye (Lond) 2011 Apr;25(4):489-493.
- 53. Mitra S, Chayani N, Mohapatra D, Barik MR, Sharma S, Basu S. High prevalence of biofilm-forming MRSA in the conjunctival flora in chronic dacryocystitis. Semin Ophthalmol 2019;34(2):74-79.
- 54. Rameshkumar G, Ramakrishnan R, Shivkumar C, Meenakshi R, Anitha V, Venugopal Reddy YC, et al. Prevalence and antibacterial resistance patterns of extended-spectrum beta-lactamase producing Gram-negative bacteria isolated from ocular infections. Indian J Ophthalmol 2016 Apr;64(4):303-311.
- 55. Eguchi H, Miyamoto T, Kuwahara T, Mitamura S, Mitamura Y. Infectious conjunctivitis caused by Pseudomonas aeruginosa isolated from a bathroom. BMC Res Notes 2013 Jul;6(1):245.
- 56. Dave A, Samarth A, Karolia R, Sharma S, Karunakaran E, Partridge L, et al. Characterization of Ocular Clinical Isolates of Pseudomonas aeruginosa from Non-Contact Lens Related Keratitis Patients from South India. Microorganisms 2020 Feb;8(2):260.
- 57. Hilliam Y, Kaye S, Winstanley C. Pseudomonas aeruginosa and microbial keratitis. J Med Microbiol 2020 Jan;69(1):3-13.
- 58. Al-Mujaini AS. Knowledge, attitudes and practices related to common eye diseases among the Omani population: how far have we come. Oman Med J 2020 Jan;35(1):e96.