A 45-year-old woman, controlled diabetic and hypertensive, presented with a complaint of a painless nodule on her left shin for the last three months which had gradually increased in size since she noticed it. There was no history of exposure to sunlight, itching, or trauma. Her garments had always covered her thighs and legs. On examination, there was a single, 3.8 × 2.9 × 1.4 cm, non-tender, purplish-pink, non-ulcerative, nodular lesion over the pretibial region of the middle one-third of the left leg. There was a rim of 4–6 mm skin discoloration all around [Figure 1]. The lesion was freely mobile over the underlying bone. There were no satellite lesions and no lymphadenopathy in the popliteal fossa and groin. The rest of the leg appeared normal with no functional or distal neurovascular deficit. Routine blood test results were within normal range while radiologic investigations revealed no signs suggestive of bony invasion.
 Figure 1: Clinical photograph showing the nodular lesion over the middle one-third of the left shin. (pretibial region).
Figure 1: Clinical photograph showing the nodular lesion over the middle one-third of the left shin. (pretibial region).
Question
1- What is the most likely diagnosis?
a. Nodular melanoma.
b. Basal cell carcinoma.
c. Leukemia cutis.
d. Merckel cell carcinoma.
Answer
b. Basal cell carcinoma.
An incisional wedge biopsy was taken from the edge of the lesion incorporating the adjacent normal healthy skin as well. It revealed a nodular-cystic variety of basal cell carcinoma (BCC). The lesion was surgically excised. Although there are no universally accepted guidelines for extent of margins of excision, 1.5 cm of clinically healthy skin all around the lesion was included to ensure clear margins for such high-risk BCC [Figures 2 and 3]. The resultant defect was resurfaced with an intermediate-thickness split skin graft. On histopathological examination, hematoxylin and eosin-stained sections showed basaloid tumor cells arising from the epidermis, arranged in nests and small islands [Figure 4a]. Peripheral palisading of round to oval tumor cells was seen [Figure 4b]. The cells comprised of basophilic nuclei, inconspicuous nucleoli, scant cytoplasm, mild pleomorphism, and occasional mitosis. Fibromyxoid stroma was seen around the tumor while no neurovascular invasion was noted. The diagnosis of BCC was confirmed. All lateral and deep resected margins were free of the tumor. The patient remained recurrence-free till her last follow-up one year after surgery.
 Figure 2: Intraoperative picture showing the defect after tumor resection with 1.5 cm margins.
Figure 2: Intraoperative picture showing the defect after tumor resection with 1.5 cm margins.
 Figure 3: The excised specimen with sutures marked for orientation.
Figure 3: The excised specimen with sutures marked for orientation.
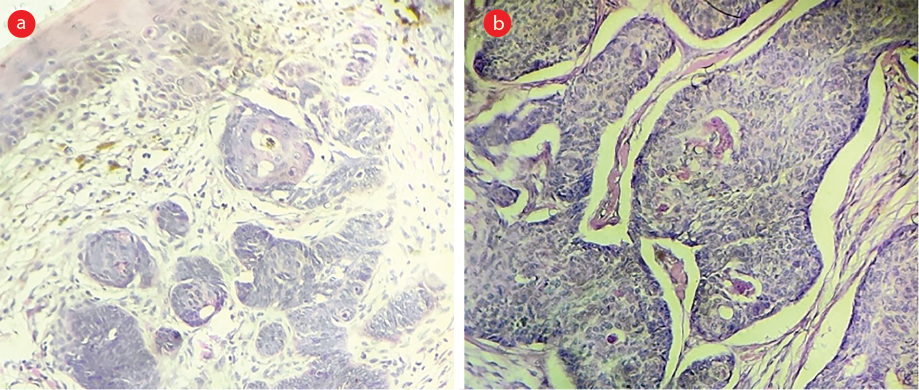 Figure 4: (a) Hematoxylin and eosin stain showing tumor arising from epidermis with basaloid tumor cells arranged in nests and small islands, magnification = 40 ×. (b) Photomicrograph showing peripheral palisading of round to oval tumor cells, magnification = 200 ×.
Figure 4: (a) Hematoxylin and eosin stain showing tumor arising from epidermis with basaloid tumor cells arranged in nests and small islands, magnification = 40 ×. (b) Photomicrograph showing peripheral palisading of round to oval tumor cells, magnification = 200 ×.
Clinical variants of BCC include nodular, cystic, pigmented, morpheaform, superficial, and infiltrative types with specific histological features. Certain adnexal tumors like trichoepithelioma, trichoblastoma, sebaceous carcinoma, adenoid cystic carcinoma, basaloid follicular hamartoma, and Merkel cell carcinoma can also mimic BCC on histology which may require immunohistochemistry for a definite diagnosis.1
As per the National Comprehensive Cancer Network (NCCN) guidelines version 2.2021, any BCC lesion on the pretibial region is considered high risk, irrespective of size.2 Lesions on the feet (as they tend to be sun-exposed) are also considered high risk. The rest of the extremities are considered low risk unless the lesion is > 2 cm. This is a change from the previous versions of NCCN Guidelines, which comprised risk stratification into ‘H’, ‘M’, and ‘L’ zones.3 Pretibial lesions were included in the ‘M zone’ and were considered high-risk only if > 10 mm. The modification in risk stratification in the NCCN guidelines is a desirable change as it ensures that the primary lesion itself is treated as a high-risk lesion, thereby treating it aggressively with wider surgical margins minimizing the risk of recurrence.
BCC lesions on the legs are more frequently seen in women, possibly due to greater sun exposure attributed to a lack of protective clothing.4 However, our patient always kept her legs covered as per the tradition in India. As early as 1957, Clark and Mavor noted that the pretibial region, especially in women, tended to be poorly protected by clothing, leading to minor injuries and swellings which often would be unnoticed or dismissed as hematomas.5 They described three cases of neglected pretibial lesions in young women which were found to be malignant (though not BCC) and suggested that the predisposition to trauma might be further compounded by relative lack of subcutaneous tissue and fusion of deep fascia with the anterior and medial borders of the tibia.5 Additionally, poor vascularity of the pretibial region makes it prone to delayed healing and breakdowns.
While BCC frequently occurs in the head and neck region,6 its occurrence over the leg is extremely uncommon, especially if there has been no exposure to sunlight. Due to the paucity of the subcutaneous fat in the pretibial region, there can be rapid invasion and destruction of the underlying bone (rodent ulcer). Such neglected lesions may require amputation and inguinal block dissection leading to increased morbidity. BCC has also been described to develop in recurrent erysipelas and chronic lymphedema in the leg.7
Thus, clinicians must maintain a high index of suspicion so as to not miss early detection of the BCC lesions even in non-sun exposed areas during routine checkups. Several cases are often diagnosed late as they remain unnoticed under clothing or are initially mistaken to be benign skin changes. Moreover, women who habitually keep their legs covered may feel shy to get them examined by male doctors. All suspicious lesions on the pretibial region must be biopsied and treated as high-risk if diagnosed as BCC.
Disclosure
The authors declared no conflicts of interest. A written consent was taken from the patient.
references
- 1. Stanoszek LM, Wang GY, Harms PW. Histologic mimics of basal cell carcinoma. Arch Pathol Lab Med 2017 Nov;141(11):1490-1502.
- 2. National Comprehensive Cancer Network. Basal cell skin cancer v.2.2021. [cited 2022 November 26]. Available from: https://www.nccn.org/guidelines/guidelines-detail?category=1&id=1416.
- 3. National Comprehensive Cancer Network. Basal cell skin cancer v.1.2020. [cited 2022 November 26]. Available from: https://www.nccn.org/guidelines/guidelines-process/transparency-process-and-recommendations/GetFileFromFileManager?fileManagerId=6863.
- 4. Carlson KC, Connolly SM, Winkelmann RK. Basal cell carcinoma on the lower extremity. J Dermatol Surg Oncol 1994 Apr;20(4):258-259.
- 5. Clark CG, Mavor GE. Pretibial lesions. Br Med J 1957 Sep;2(5045):625-626.
- 6. Forae GD, Olu-Eddo AN. Malignant skin tumors in Benin City, South-South, Nigeria. Oman Med J 2013 Sep;28(5):311-315.
- 7. Lotem M, Tamir G, Loven D, David M, Hauben D. Multiple basal cell carcinomas of the leg after recurrent erysipelas and chronic lymphedema. J Am Acad Dermatol 1994 Nov;31(5 Pt 1):812-813.