Many kidney diseases in children can be diagnosed and treated without histopathological confirmation. However, kidney biopsy may be indicated for glomerular, interstitial, and vascular conditions such as steroid-resistant nephrotic syndrome, lupus nephritis, and vasculitis. A retrospective study in Morocco showed that the most common indication for kidney biopsy in adolescents > 16 years was a nephrotic syndrome with hematuria and/or renal failure.1 A systematic review of 17 studies from seven Arab countries revealed the commonest type of primary glomerular disease among children in the region to be minimal change disease (MCD) (29.25%), followed by focal segmental glomerulosclerosis (FSGS) (22.34%).2 In Oman, a study based on light microscopy and immunofluorescence conducted in a tertiary hospital among all age groups showed that FSGS (21.1%) was the most common primary glomerular disease.3 Our population has a high rate of consanguinity which increases the incidence of inherited kidney diseases.
To our knowledge, no study has been conducted in Oman focusing on the clinical indications and outcomes of pediatric renal biopsies. Therefore, we aimed to determine the spectrum of kidney diseases in below-13-year-old children in Oman and evaluate the outcomes and complications of kidney biopsy among them.
Methods
This retrospective study was conducted in the pediatric nephrology unit of the Child Health Department at Royal Hospital, Muscat, one of the two tertiary hospitals in Oman performing kidney biopsies. The study included all children aged < 13 years who underwent kidney biopsies at Royal Hospital between January 2014 and June 2019. The study was approved by the Royal Hospital ethical committee (Ref. 85/2019).
Cases of kidney biopsies taken for investigating renal masses, nephrectomies, and pyeloplasties were excluded from the study. Data retrieved from the hospital database included patient demographics, clinical findings at presentation, laboratory results, renal biopsy findings, and post-biopsy complications. Most biopsies were performed by interventional radiologists under ultrasound guidance and a few by pediatric nephrologists. Two (2.6%) cases were open biopsies done by pediatric surgeons.
The hospital protocol for kidney biopsy requires the pediatric patient to be admitted one day before the procedure. Baseline laboratory investigations are conducted including full blood count, renal function, electrolytes, coagulation profile, and blood for crossmatch. Further laboratory investigations depend upon the clinical condition of the child. Consent for the biopsy is taken from the parent or guardian. The patient is reviewed by the anesthesiologist and kept nil per oral as per the anesthesiologist’s instructions. Kidney biopsies are performed under general anesthesia aided by real- time ultrasound using a GE ultrasound machine—either Logic Er7 or S8 with either 1-5 curvilinear probe or 9 L sector probe according to the weight of the child. The biopsy is taken from the lower pole of the left kidney using 18-gauge needle using manual true cut or biopsy gun (Magnum-Bard). The left kidney is preferred as it is positioned lower than the right kidney; and hence, more easily accessible. After the procedure, the patient is transferred to the pediatric ward and closely monitored for 24 hours for complications.
Three core biopsies are then sent to the histopathology laboratory for light microscopy, immunofluorescence, and electron microscopy (EM). The specimen is sectioned at 4 microns thickness, processed and stained using hematoxylin, eosin, periodic acid-Schiff, and methenamine silver stains. One slide is stained for elastic Van Gieson and one for Masson trichrome. Immunofluorescence is done by direct method on frozen tissue and stained for immunoglobulin G (IgG), IgA, IgM, C3, C1q, fibrinogen, kappa, and lambda. Biopsies are read by one of two renal pathologists either at Royal hospital or at Sultan Qaboos University Hospital, also in Muscat.
We compiled the retrieved patient data using EpiData software Version 4.6 which was released by “The EpiData Association” Odense, Denmark. Statistical analyses were performed using SPSS (IBM Corp. Released 2011. IBM SPSS Statistics for Windows, Version 20.0. Armonk, NY: IBM Corp.). The frequencies and percentages of all variables were calculated.
Results
The subjects were comprised of 78 children (39 girls and 39 boys) with a median age of 8.0 years (range = 0–13 years) on the day of biopsy. Their mean weight was 25.5 kg±12.9. At presentation, 70 (89.7%) patients had proteinuria, 31 (39.7%) had microscopic hematuria, and 12 (15.4%) had gross hematuria. Abnormal glomerular filtration rate was found in 34 (43.6%) patients and hypertension in 26 (33.3%). Fourteen (17.9%) patients had systemic manifestations including skin rash, oral ulcers, and joint pain [Table 1].
Table 1: Patient demographics and presenting symptoms.
|
Total patients
|
78
|
100
|
|
Sex
|
|
|
|
Male
|
39
|
50.0
|
|
Female
|
39
|
50.0
|
|
Age, years
|
|
|
|
< 3
|
7
|
9.0
|
|
3–5
|
19
|
24.4
|
|
6–13
|
52
|
66.7
|
|
Mean age ± SD
|
7.2 ± 3.3
|
|
|
Median age
|
8.0
|
|
|
Clinical manifestations
|
|
Proteinuria
|
70
|
89.7
|
|
Abnormal GFR
|
34
|
43.6
|
|
Microscopic hematuria
|
31
|
39.7
|
|
Hypertension
|
26
|
33.3
|
|
Systemic manifestation
|
14
|
17.9
|
GFR: glomerular filtration rate.
Figure 1 graphically depicts the regional distribution of patients between the governorates in Oman. Two of the 78 patients were non-Omani.
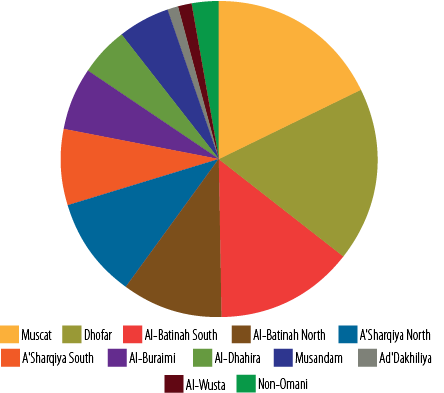 Figure 1: Regional distribution of children in Oman who underwent kidney biopsies (N = 78).
Figure 1: Regional distribution of children in Oman who underwent kidney biopsies (N = 78).
Seventy (89.7%) biopsies were taken from native kidneys and eight (10.3%) from transplanted kidneys. Indications for biopsies of transplanted kidneys were BK polyomavirus viremia with allograft dysfunction in four patients and allograft dysfunction with negative virology in the remaining four. All the renal biopsies underwent a histopathological examination by light microscopy. EM report was not available for 27 (34.6%) cases and immunofluorescence was not done for two (2.6%) cases.
MCD was the most common diagnosis as revealed by renal biopsy in our patients, accounting for 15 (19.2%) cases. Lupus nephritis and FSGS, the second most common finding, were present in 13 (16.7%) patients each. Of the children with lupus nephritis, 11 were female and two were male. Class II lupus nephritis was seen in one patient, while class III and IV were seen in three and nine patients respectively [Table 2].
Table 2: Diagnostic findings from kidney biopsies in children in Oman (N = 78).
|
Minimal change disease
|
15
|
19.2
|
|
Focal segmental glomerulosclerosis
|
13
|
16.7
|
|
Lupus nephritis
|
13
|
16.7
|
|
Hereditary nephropathy.
|
10
|
12.8
|
|
Complications of kidney transplant
|
8
|
10.3
|
|
Post-infectious glomerulonephritis
|
3
|
3.8
|
|
Thrombotic microangiopathy
|
3
|
3.8
|
|
Membranoproliferative glomerulonephritis and C3 glomerulopathy
|
2
|
2.6
|
|
Acute tubular necrosis
|
2
|
2.6
|
|
Membranous nephropathy
|
1
|
1.3
|
|
Finnish type nephrotic syndrome.
|
1
|
1.3
|
|
Pyelonephritis
|
1
|
1.3
|
|
Normal
|
3
|
3.8
|
|
Inconclusive
|
4
|
5.1
|
Hereditary nephropathy (Alport syndrome/nephronophthisis) accounted for 10 (12.8%) cases. Post-infectious glomerulonephritis and thrombotic microangiopathy (TMA) were present in three (3.8%) each. Two patients with TMA were diagnosed to have atypical hemolytic uremic syndrome while the other patient had features of TMA in addition to chronic changes in the biopsy findings and was diagnosed with familial FSGS. Membranoproliferative glomerulonephritis and C3 glomerulopathy were found in two (2.6%) children while another two had acute tubular necrosis. Membranous nephropathy, Finnish type nephrotic syndrome, and chronic pyelonephritis accounted for one (1.3%) each. Four of transplanted kidney biopsies were reported as BK polyomavirus nephropathy, two as acute rejection, and one each as cases of chronic rejection and calcineurin inhibitor toxicity. Only three (3.8%) biopsies were reported as normal [Table 2]. The indication of kidney biopsy from these three patients was microscopic hematuria. Two biopsies did not undergo EM, while one EM sample contained only medullary tissue without glomeruli. Reports on four (5.1%) biopsies were diagnostically inconclusive or insufficient [Table 2].
Twenty-one patients (26.9%) had genetic studies performed: one of them was found to have congenital nephrotic syndrome secondary to NPHS1 mutation, three had familial nephrotic syndrome secondary to NPHS2 mutation, and two had whole exome sequencing conducted abroad, which confirmed our diagnosis of nephronophthisis.
The most common complications following renal biopsy were pain requiring analgesia in 38 (48.7%) and gross hematuria in 10 (12.8%) patients [Table 3]. There was no case of severe hematuria requiring blood transfusion or surgical intervention. Arteriovenous fistula, urinomas, or death following biopsy were not seen in our cohort. For transplant patients also, major complications such as arteriovenous fistula, graft infection, or loss of graft did not occur—only mild ones such as gross hematuria and pain which responded to analgesia. Most complications occurred in the first eight hours after the procedure and the majority improved and were discharged within 24 hours.
Table 3: Prevalence of post-biopsy complications in children (N = 78).
|
Pain that required analgesic
|
38
|
48.7
|
|
No complications
|
34
|
43.6
|
|
Gross hematuria
|
10
|
12.8
|
Some patients had more than one post-biopsy complication.
Discussion
To our knowledge, this is the first study in Oman addressing cases of kidney biopsies in children. We found that the most common biopsy-based diagnosis in our patients was MCD (19.2%), followed by lupus nephritis (16.7%) and FSGS (16.7%). A study conducted in Oman between 1999 and 2010 on the pattern of glomerular diseases based on light microscopy and immunofluorescence for adult and pediatric patients showed that lupus nephritis was the most common glomerular disease (30.4%) followed by FSGS (21.1%) and then MCD (17%).3 A retrospective study in children in Saudi Arabia found that MCD was the most common histopathological finding (25%), followed by mesangial proliferative glomerulonephritis (15.7%).4 A systematic review of 17 studies to determine the incidence of pediatric glomerular diseases in the Arab world from 1990 to 2018 revealed that lupus nephritis comprised 36.1% of all cases, followed by MCD at 29.3% then FSGS at 22.3%.2 Data from around the world showed a high prevalence of membranoproliferative glomerulonephritis in developing countries compared to the high prevalence of IgA-nephropathy and MCD in more developed countries.5 MCD was the most common histopathological diagnosis in most of the above-mentioned studies4,5 and not lupus nephritis and FSGS, which agree with our findings.
The relatively lower prevalence of MCD in our sample may be explained by the inclusion of fewer cases with nephrotic syndrome. Kidney biopsy in children with nephrotic syndrome limited to steroid dependency, or frequent relapsing nephrotic syndrome before starting calcineurin inhibitor. Genetic studies for steroid- resistant nephrotic syndrome were performed for 19 patients of whom four were found to have a relevant mutation. However, as not all genes responsible for familial FSGS were tested for at our center, the latter cannot be ruled out in children who were negative for NPHS1 and NPHS2 genes.
Most of our patients were older than six years, which can be explained by the fact that secondary renal diseases like lupus and FSGS due to immune dysregulation are more common in older children. Younger children are likely to have congenital and hereditary renal disease which can be diagnosed by imaging and genetic studies. A previous study on chronic kidney disease in Omani children reported that the most common etiologies were congenital anomalies of kidney and urinary tract followed by hereditary renal disease.6 Their median age at diagnosis of chronic kidney disease was two years and 61% of those children were below three years at diagnosis. 6
Non-nephrotic range proteinuria and nephrotic syndrome were the most common indications for renal biopsy in our patients as also seen in other studies.5 Studies from Turkey and Italy showed that the most frequent indication for pediatric renal biopsy was nephrotic syndrome followed by non-nephrotic range proteinuria.7,8
Percutaneous real-time ultrasound-guided renal biopsy, despite being recognized as safe in children, carries risk of complications such as gross hematuria, perirenal hematoma, arteriovenous fistulas, infection, damage to adjacent organs, or even loss of the kidney.7 In all our cases, renal biopsy was conducted safely and effectively, albeit with a few minor complications such as pain requiring analgesia and gross hematuria that did not require blood transfusion nor surgical intervention. A study in Oman showed an incidence of complications following renal biopsy of 10% with most of them being procedure-related bleeding.9 A study from Saudi Arabia had results similar to ours, with severe pain at the biopsy site as the most common complication (10.2%) followed by gross hematuria (2.8%).4 Another study from Germany in 295 children and adolescents who underwent a total of 438 ultrasound-guided kidney biopsies over 14 years period, there were 18 ( 4.1%) cases of complication; six of these patients required cystoscopy or angiography, three patients received blood transfusion, but no major complication that required surgical intervention occurred.10
The limitations of this study include its retrospective nature which involved past data which were sometimes incomplete. With only 78 cases, our sample size was small, and the follow-up periods tended to be short. Suggestions for future studies are to include a larger sample size involving other centers in Oman, as well as covering the neighboring Arabian Gulf nations with similar ethnicities. Future studies should also cover kidney biopsy cases over longer periods. Such studies will help pediatricians and pediatric nephrologists to be aware of the spectrum of kidney diseases among children in the region and to evaluate the outcome and complications of kidney biopsy in these children.
Conclusion
Common histopathological findings in Omani children who underwent kidney biopsy were MCD followed by lupus nephritis and FSGS. The main complication of kidney biopsy was pain that responded to analgesics, followed by gross hematuria that did not require blood transfusion. There were no serious post-biopsy complications. Our findings may also be useful to healthcare providers assigned to counsel children and parents before kidney biopsy.
Disclosure
The authors declared no conflicts of interest. No funding was received for this study.
references
- 1. Souilmi FZ, Houssaini TS, Alaoui H, Harmouch T, Atmani S, Hida M. Indications and results of renal biopsy in children: a single-center experience from Morocco. Saudi J Kidney Dis Transpl 2015 Jul-Aug;26(4):810-815.
- 2. Alwahaibi NY, Al Issaei HK, Al Dhahli BS. Incidence of pediatric glomerular diseases in Arab world: a systematic review. Saudi J Kidney Dis Transpl 2019 Jan-Feb;30(1):15-23.
- 3. Alwahaibi NY, Alhabsi TA, Alrawahi SA. Pattern of glomerular diseases in Oman: a study based on light microscopy and immunofluorescence. Saudi J Kidney Dis Transpl 2013 Mar;24(2):387-391.
- 4. Al Menawy L, Amuosi J, Ramprasad KS, Shaheen FA. Percutaneous renal biopsy and its findings in children and adolescents in saudi arabia: a single center experience. Saudi J Kidney Dis Transpl 1997 Jul-Sep;8(3):289-293.
- 5. Fiorentino M, Bolignano D, Tesar V, Pisano A, Van Biesen W, D’Arrigo G, et al; ERA-EDTA Immunonephrology Working Group. Renal biopsy in 2015–from epidemiology to evidence-based indications. Am J Nephrol 2016;43(1):1-19.
- 6. Al Riyami MS, Al Shehhi M, Al Sulaimi T, Al Mamary L, Al Maskari A, Al Ghaithi B, et al. Epidemiology and outcome of CKD in Omani children. Kidney Int Rep 2019 Feb;4(5):727-732.
- 7. Demircin G, Delibaş A, Bek K, Erdoğan O, Bülbül M, Baysun S, et al. A one-center experience with pediatric percutaneous renal biopsy and histopathology in Ankara, Turkey. Int Urol Nephrol 2009 Dec;41(4):933-939.
- 8. Santangelo L, Netti GS, Giordano P, Carbone V, Martino M, Torres DD, et al. Indications and results of renal biopsy in children: a 36-year experience. World J Pediatr 2018 Apr;14(2):127-133.
- 9. Al Riyami D, Al Shaaili K, Al Bulushi Y, Al Dhahli A, Date A. The spectrum of glomerular diseases on renal biopsy: data from a single tertiary center in oman. Oman Med J 2013 May;28(3):213-215.
- 10. Franke M, Kramarczyk A, Taylan C, Maintz D, Hoppe B, Koerber F. Ultrasound-guided percutaneous renal biopsy in 295 children and adolescents: role of ultrasound and analysis of complications. PLoS One 2014 Dec;9(12):e114737.