Congenital cholesteatoma (CC) is an expanding cystic mass of keratinizing squamous epithelium located behind an intact tympanic membrane. Though it is present at birth, it is usually diagnosed during infancy or early childhood. It represents epidermoid cells that failed to involute, and these cells grow gradually to become clinically apparent later in childhood.1 Though it is commonly located intracranially, at extracranial sites, it is often seen in the anterior superior quadrant of the mesotymapnum.2 However, hypotympanum is a very unusual site for CC and, to date, only one case has been reported in the English literature in a 16-year-old boy with Treacher Collins syndrome.3 CC may present as asymptomatic white mass behind an intact tympanic membrane or in 82% of cases incidentally found during routine otoscopy, imaging, or a procedure like myringotomy.4
The treatment of choice in the management of CC is complete surgical excision, which nowadays is often performed endoscopically if it is small and localized. However, hidden sites (e.g., sinus tympani, facial recess, anterior tympanic sinus, and hypotympanum) are often difficult to access and there is a high chance of recurrence if not completely excised.5
We are reporting the first case report of a successful endoscopic-assisted infracochlear hypotympanotomy approach for the excision of a large hypotympanic CC with extension into the jugular foramen and the carotid canal.
Case report
A 13-year-old girl presented to our outpatient department with complaints of decreased hearing, on and off earache, and discharge from her right ear for the last five years. The discharge was foul-smelling in nature and was intermittently blood-stained for the last year. She was treated as a case of otitis media at a local hospital in the form of antibiotics and decongestants, but there was a partial response to the treatment. There was no history of any otological surgical procedure. On examination of the right ear, the pinna and the external auditory canal were normal. On otoscopy, the right tympanic membrane was congested, and there was a bulge in the anteroinferior quadrant while the left side pars tensa was grade 2 retracted. Pure tone audiometry showed a mild conductive hearing loss on both sides, and the tympanometry was type B on the right and type C on the left side. High-resolution computed tomography (CT) of temporal bone showed a large homogenous soft tissue density in the right hypotympanum with erosion base of the skull and widening of the jugular foramen [Figure 1]. The fallopian canal and ossicular chain were intact on the right side. Contrast-enhanced magnetic resonance imaging (MRI) showed a 2.1 × 1.1 × 1.2 cm non-enhancing mass in the right hypotympanum with extension into the right jugular foramen with erosion of its anterior wall, close abutment of the right jugular bulb and the petrous part of the right internal carotid artery [Figure 2]. It was hyperintense on T2, heterogeneously hyperintense on fluid-attenuated inversion recovery, and hypointense on T1, suggesting a diagnosis of cholesteatoma.
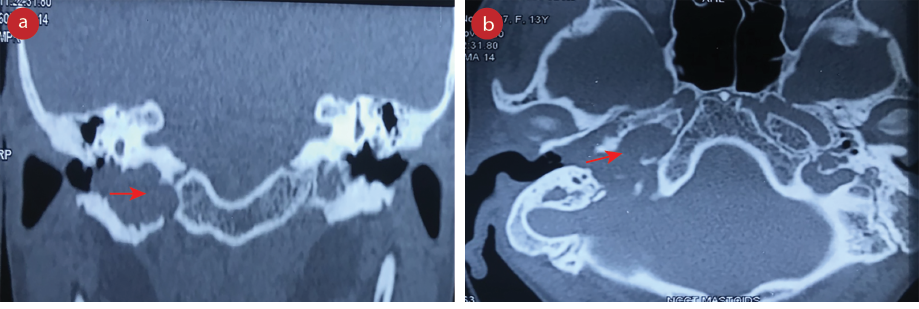 Figure 1:(a) High-resolution CT scan of temporal bone coronal cut showing a large homogenous soft tissue density in right hypotympanum (red arrow) with extension into the jugular foramen. (b) High-resolution CT scan of temporal bone axial cut showing a large homogenous soft tissue density in right hypotympanum (red arrow) with extension into the jugular foramen and carotid canal.
Figure 1:(a) High-resolution CT scan of temporal bone coronal cut showing a large homogenous soft tissue density in right hypotympanum (red arrow) with extension into the jugular foramen. (b) High-resolution CT scan of temporal bone axial cut showing a large homogenous soft tissue density in right hypotympanum (red arrow) with extension into the jugular foramen and carotid canal.
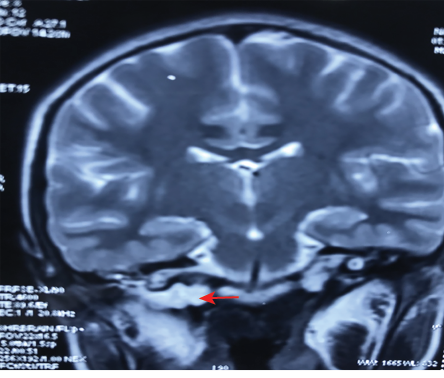 Figure 2: Coronal cut of MRI T2-weighted image showing a hyperintense expansile mass lesion in the right hypotympanum with its extension into the petrous part of the internal carotid artery
Figure 2: Coronal cut of MRI T2-weighted image showing a hyperintense expansile mass lesion in the right hypotympanum with its extension into the petrous part of the internal carotid artery
(red arrow).
The patient and her parents were informed about the clinical diagnosis, management options, the possible need for second-look surgery, and follow-up imaging, and a detailed informed consent was obtained. Under general anesthesia, parts were cleaned and draped. A post-auricular incision was made, and a posteriorly based extended tympanomeatal flap from 6 to 2 o'clock was elevated, and the tympanic membrane was reflected anteriorly. The middle ear was entered, and the cholesteatoma sac was visualized. Superiorly, it extended up to the cochlea and the round window; however, the inferior extent was not well-delineated. The ossicles were normal and mobile. Inferiorly, the bony floor of the external auditory was drilled to complete the hypotympanotomy, still, the anterior and inferior extent sac was not completely visualized. Then cortical mastoidectomy was performed, and the posterior bony canal wall over the vertical part of the fallopian canal was drilled to the thin paper bony remnants over the nerve to access the posterior extent of the sac. The anterior wall of the bony canal was drilled along with part of the mastoid tip to access the jugular bulb. The cholesteatoma sac was occupying the hypotympanum, inferiorly adherent to the jugular bulb and anteriorly it was extending up to the bony carotid canal, which was partly dehiscent. Finally, the sac was decompressed and carefully elevated from the cavity. Under the microscope, the posterior extent of the sac was difficult to visualize, so a 2.7 mm 30 degree rigid scope was used. During the elevation of the matrix, there was a tear in the dura of size around 1.5 cm. The cerebrospinal fluid (CSF) leak was controlled with pressure with gel foam, and once the matrix is completely removed under the endoscope, the tear is packed with muscle, temporalis fascia, and fibrin glue. Multiple pieces of cartilage were used to fill the cavity and a fascia graft was kept in the cavity. Postoperatively, the patient was kept on intravenous antibiotics and acetazolamide tablets to reduce CSF pressure. She was on absolute bed rest for a week and the medicated pack was removed on day 10. There was no CSF leak, and she was discharged on oral antibiotics and kept on follow-up. Histopathology confirmed the diagnosis of cholesteatoma and a repeat MRI after six months did not show any recurrence of the disease [Figure 3]. The patient is doing well and is symptom-free.
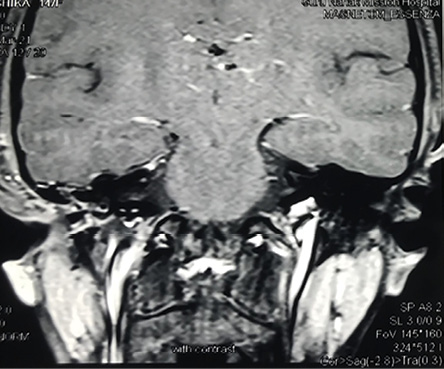 Figure 3: Post-surgery MRI coronal cut showing no residual disease.
Figure 3: Post-surgery MRI coronal cut showing no residual disease.
Discussion
CC is a rare disease and is around 2–5% of all cholesteatomas.6 Strict criteria for diagnosis of CC have been suggested including a whitish mass present in the middle ear cavity with normal tympanic membrane, no history of otorrhea or perforation, and no history of otological surgery. History of otitis media is not an exclusion for the disease.7 Most such cases are either asymptomatic, incidentally found on imaging, or seen during surgery. It enlarges gradually, but as cellular activity is high in the pediatric age group, they grow faster than adults, and present at any age from infancy to adult (mean age = 16.7 years).8 Our patient was symptomatic for five years and presented at age 13, this could be due to hidden site hypotympanum and it continued to expand inferior-medially.
Radiology plays an important role in the diagnosis and follow-up of CC cases. It not only helps in delineating the location and extent of the disease but also in visualizing hidden areas (e.g., sinus tympani, hypotympanum, and cerebellopontine angle). Preoperative high-resolution CT is a must especially when we are suspecting complications of otitis media or a case of CC.9 But it is not very helpful in the postoperative assessment of recurrence of disease and differentiating from granulation tissue. In 2005, a report published that post-contrast T1-weighted MRI effectively differentiates between these two, as cholesteatoma is an avascular structure; hence, it does not enhance on contrast while granulation tissue being vascular, enhances in late phase (40–45 minutes) images.10 However, its failure to diagnose cholesteatoma < 3 mm and the long duration taken for imaging makes a diffusion-weighted image (DWI) MRI the investigation of choice.9 In our case, the preoperative CT scan showed a large soft tissue density in the middle ear, hypotympanum, thinning of the tegmen tympani, along with destruction of the jugular foramen and base of the skull [Figure1]. MRI showed a 21 × 11 × 12 mm sized lesion that was hypointense on T1, hyperintense on T2, heterogeneously hyperintense on fluid-attenuated inversion recovery, restricted diffusion on DWI in the right hypotympanum with the erosion of anterior wall of right jugular foramen, and close abutment of jugular bulb and petrous part of the internal part of carotid artery. All these findings were consistent with a diagnosis of cholesteatoma.
CC usually presents in a healthy ear with no prior history of infection and normal eustachian tube function. In addition, in comparison to acquired cholesteatoma, it is often a sac-like confined structure making it more completely excisable. The goal of CC surgery is disease clearance with preservation or restoration of hearing. Traditionally, it has been done under a microscope, but with wide-angle view and easy visualization of hidden area endoscopes has gained popularity.11 Mann et al,3 reported a case of hypotympanum cholesteatoma in a 16- year-old boy with Treacher Collins syndrome, which was excised by an extended hypotympanotomy infracochlear approach. The patient had multiple surgeries performed for the mandibular fossa reconstruction in early childhood, raising doubt about the congenital nature of cholesteatoma.
Rigid endoscopes are increasingly being used in the excision of cholesteatoma, initially as an adjunct to microscopes to look for any residual disease. However, they are used in limited staged CC.12 Endoscopes have advantages of better, wider, and clear images and are quite useful in the visualization of hidden areas where microscopic examinations are cumbersome. When used as an adjunct to microscopic surgery at the end of surgery to look for any residual disease, it reduces the incidence of residual cholesteatoma from 47–6%.13 In our case, an angled scope was used to delineate the posterior extent of the sac, removal of matrix from vital area (e.g., dura and carotid canal area). Again, it was useful in localizing the site and closing the defect of the CSF leak.
Conclusion
CC should be a differential diagnosis in persistent, refractory cases of pediatric otitis media and DWI MRI is the imaging of choice. The CC of hypotympanum extending to the jugular foramen and carotid canal is a rare entity, and the endoscopic-assisted infracochlear hypotympanotomy approach is safe and effective for its excision.
Disclosure
The authors declared no conflicts of interest. A detailed informed consent was obtained from the patient and her parents.
references
- 1. Mahanta VR, Uddin FJ, Mohan S, Sharp JF. Non-classical presentation of congenital cholesteatoma. Ann R Coll Surg Engl 2007 Mar;89(2):W6-W8.
- 2. Abdel-Aziz M. Congenital cholesteatoma of the infratemporal fossa with congenital aural atresia and mastoiditis: a case report. BMC Ear Nose Throat Disord 2012 Jun;12:6.
- 3. Mann W, Al-Nawas B, Wriedt S, Mann S, Koutsimpelas D. Cholesteatoma of the hypotympanum in a patient with Treacher Collins syndrome. Auris Nasus Larynx 2014 Feb;41(1):101-104.
- 4. McGill TJ, Merchant S, Healy GB, Friedman EM. Congenital cholesteatoma of the middle ear in children: a clinical and histopathological report. Laryngoscope 1991 Jun;101(6 Pt 1):606-613.
- 5. Kuczkowski J, Narozny W, Mikaszewski B. Congenital cholesteatoma with external ear canal anomalies. Otol Neurotol 2007;28(5):725-726.
- 6. Stapleton AL, Egloff AM, Yellon RF. Congenital cholesteatoma: predictors for residual disease and hearing outcomes. Arch Otolaryngol Head Neck Surg 2012 Mar;138(3):280-285.
- 7. Levenson MJ, Michaels L, Parisier SC. Congenital cholesteatomas of the middle ear in children: origin and management. Otolaryngol Clin North Am 1989 Oct;22(5):941-954.
- 8. Kojima H, Tanaka Y, Shiwa M, Sakurai Y, Moriyama H. Congenital cholesteatoma clinical features and surgical results. Am J Otolaryngol 2006 Sep-Oct;27(5):299-305.
- 9. Schwartz KM, Lane JI, Bolster BD Jr, Neff BA. The utility of diffusion-weighted imaging for cholesteatoma evaluation. AJNR Am J Neuroradiol 2011 Mar;32(3):430-436.
- 10. Ayache D, Williams MT, Lejeune D, Corré A. Usefulness of delayed postcontrast magnetic resonance imaging in the detection of residual cholesteatoma after canal wall-up tympanoplasty. Laryngoscope 2005 Apr;115(4):607-610.
- 11. Marchioni D, Alicandri-Ciufelli M, Piccinini A, Genovese E, Monzani D, Tarabichi M, et al. Surgical anatomy of transcanal endoscopic approach to the tympanic facial nerve. Laryngoscope 2011 Jul;121(7):1565-1573.
- 12. Park JH, Ahn J, Moon IJ. Transcanal endoscopic ear surgery for congenital cholesteatoma. Clin Exp Otorhinolaryngol 2018 Dec;11(4):233-241.
- 13. Kozin ED, Gulati S, Kaplan AB, Lehmann AE, Remenschneider AK, Landegger LD, et al. Systematic review of outcomes following observational and operative endoscopic middle ear surgery. Laryngoscope 2015 May;125(5):1205-1214.