A19-month-old boy presented with a two-week history of arching of the back while walking, which progressed to the inability to bear weight followed by the inability to sit. His mother noticed he was screaming in pain whenever she changed his diaper. He had no history of fever, chronic cough, travel, animal exposure, drinking unpasteurized milk, or sick contacts. His immunization was up to date. He had been sitting and walking since seven and 11 months old, respectively.
On physical examination, he was afebrile, and all his vital signs were within normal limits. He was keeping his leg flexed and externally rotated bilaterally. He had a normal tone and reflexes in all his extremities. There was no apparent erythema, swelling, or tenderness in his lower limbs. No restriction of movement of both the knee and hip joints. He was refusing to bear weight on his lower limbs. The spine examination showed no skin changes, swelling, or spinal deformity. He had tenderness of the lumbosacral area on palpation. His white cell count was 12.9 × 109/L, C-reactive protein was 12 mg/L, and the X-ray of his lower limbs was reported to be normal.
Questions
- What is the most likely diagnosis?
- What is the best radiological modality of diagnosis?
- How would you manage the patient?
Answers
- Spondylodiscitis in a toddler.
- Magnetic resonance imaging (MRI) of the spine.
- Analgesia, rest, and antibiotics. Infectious disease consultation should be sought to guide the duration of antibiotics.
Discussion
Spondylodiscitis (SD) was suspected in our patient, and he was started empirically on intravenous cefazolin 50 mg/kg/dose every eight hours. The diagnosis was confirmed by MRI of the spine, which showed the collapse of the intervertebral disc at L3-L4 with fluid signal intensity in the disc, endplate irregularities, and abnormal marrow signal in L3 and L4 vertebral bodies [Figure 1]. There was also perivertebral and epidural soft tissue thickening and enhancement [Figure 2]. His blood culture and sickle cell screening were negative. He showed clinical improvement in the subsequent week and was managed with intravenous antibiotics for two weeks. He was discharged home on oral cephalexin for another six weeks. At the six-week follow-up, he was back to his baseline and was walking normally. SD is a rare bacterial infection that accounts for only 1–2% of all cases of bone and joint infections in children.1,2 It involves inflammation of one or more intervertebral disc spaces and the adjacent vertebrae.1–3 The poor awareness of this condition among pediatricians is the main cause of delayed diagnosis.4 In one study, about 50% of children with SD had a delayed diagnosis of three months.4 Early diagnosis and initiation of treatment are important to avoid devastating neurological complications and spinal deformities.3 Staphylococcus aureus is the most common cause of SD in children followed by Streptococcus pyogenes. Kingella kingae should always be considered in children less than four years old.1,5 Other pathogens should be considered in specific situations like Salmonella spp. in children with sickle cell disease, Brucella spp. in patients with a history of ingestion of unpasteurized milk or animal exposure, and Mycobacterium tuberculosis in children living in tuberculosis-endemic countries.1,3–5 Lumbar spine followed by the thoracic spine is the most commonly affected area of the spine by SD.3,5 Presentation in children is indolent and non-specific most of the time.1,4 About 50% of children present with refusal to sit, crawl, stand, or walk.1,4,5 Difficulty changing diapers is not uncommon, especially in non-ambulatory children.4 Systemic symptoms like fever are uncommon in children with SD and present in about 30% of cases. Back pain of unknown etiology is not uncommon and mainly presents in children > 28 months of age.4 Patients with SD usually have normal total white cell count and either normal or mildly elevated C-reactive protein.4 Bacterial cultures including blood and tissue if possible should be done.1,4 MRI is the best radiological modality for making the diagnosis of SD as well as for assessing treatment response and looking for neurological complications.4 Management includes rest, adequate analgesia, and anti-staphylococcal penicillin, clindamycin, or first-generation cephalosporin unless another organism has been identified.1,2 Duration of antibiotics should be guided by clinical response.5
 Figure 1: (a) Sagittal short-TI inversion recovery image shows the collapse of the intervertebral disc at L3-L4 (red arrow). Abnormal marrow signal is seen in L3 and L4 vertebral bodies. (b) Contrast-enhanced sagittal T1-weighted image demonstrates abnormal enhancement in the involved vertebrae.
Figure 1: (a) Sagittal short-TI inversion recovery image shows the collapse of the intervertebral disc at L3-L4 (red arrow). Abnormal marrow signal is seen in L3 and L4 vertebral bodies. (b) Contrast-enhanced sagittal T1-weighted image demonstrates abnormal enhancement in the involved vertebrae.
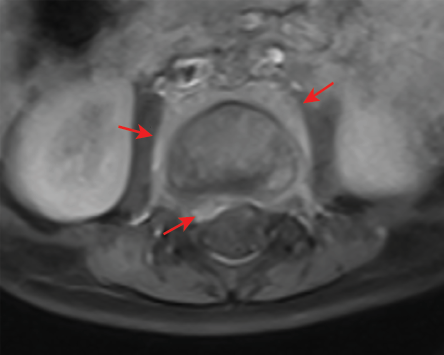 Figure 2: Contrast-enhanced axial T1-weighted image shows epidural (short arrow) and perivertebral (long arrows) soft tissue thickening
Figure 2: Contrast-enhanced axial T1-weighted image shows epidural (short arrow) and perivertebral (long arrows) soft tissue thickening
and enhancement.
Disclosure
The authors declared no conflicts of interest. A written consent was given by the father of the patient.
references
- 1. Principi N, Esposito S. Infectious discitis and spondylodiscitis in children. Int J Mol Sci 2016 Apr;17(4):539.
- 2. Saavedra-Lozano J, Falup-Pecurariu O, Faust SN, Girschick H, Hartwig N, Kaplan S, et al. Bone and joint infections. Pediatr Infect Dis J 2017 Aug;36(8):788-799.
- 3. Scheuerman O, Landau D, Schwarz M, Hoffer V, Marcus N, Hoffnung LA, et al. Cervical discitis in children. Pediatr Infect Dis J 2015 Jul;34(7):794-795.
- 4. Ferri I, Ristori G, Lisi C, Galli L, Chiappini E. Characteristics, management and outcomes of spondylodiscitis in children: a systematic review. Antibiotics (Basel) 2020 Dec;10(1):30.
- 5. Tyagi R. Spinal infections in children: a review. J Orthop 2016 Jun;13(4):254-258.