| |
Abstract
Objectives: Preterm premature rupture of membranes (PPROM) is defined as a rupture of the amniotic membranes occurring before 37 weeks of gestation and before the onset of labor. Extreme PPROM occurs prior to 26 weeks gestation and contributes to an increased risk of prematurity, leading to maternal and fetal complications. This study aims to estimate the risk factors associated with various maternal complications and to determine the worst outcomes in Omani females with extreme PPROM.
Methods: A retrospective cohort study was conducted on 44 women with extreme PPROM, who delivered at Sultan Qaboos University Hospital (SQUH) from January 2006 to December 2011. Women with incomplete information, multiple gestations, or a preterm delivery resulting from medical intervention, as well as women who delivered elsewhere were excluded from the study.
Results: Forty-four women with extreme PPROM were included in our study. The results revealed the most important risk factor to be history of infection, which was noted in 24 study participants. The mean maternal age was 30 years. The mean gestational age at PPROM and at delivery were 20.7±3.2 (range: 16-26 weeks) and 29.7±7.6 weeks (range: 17-40 weeks), respectively. The maternal complications observed in this study included; infection which was seen in 20 (45%) patients, antepartum hemorrhage in 11 (25%) patients, and cesarean section which was required in 12 (27%) patients. There was no significant association between risk factors such as gestational age at delivery, parity, maternal age at PPROM, or maternal Body Mass Index (BMI) and cesarean section rate. Infection played a major role, both as a risk factor and in causing extreme PPROM, which in turn increased in 12 patients (27%). In the multivariable model for predicting the need for cesarean section (gestational age at delivery, parity, maternal age at PPROM in years and maternal BMI), none of the factors were statistically significant.
Conclusion: Overall, concurrent infection rate was high among patients presenting with extreme PPROM. None of the baseline maternal factors predicted the need for cesarean section. This is likely due to the small sample size; hence, larger prospective studies are needed to confirm these findings.
Keywords: Extreme; PPROM; Risk Factors; Maternal Outcomes.
Introduction
The major cause of neonatal morbidity and mortality is preterm birth. It is divided into three categories; preterm premature rupture of membrane, preterm labor, and early delivery resulting from medical intervention. Preterm premature rupture of membranes (PPROM) is defined as a rupture of the amniotic membranes before 37 weeks of gestation and before the onset of labor, while extreme PPROM occurs before 26 weeks gestation. The incidence of PPROM in all pregnancies is 2-3%, and comprises 30-40% of preterm deliveries.1 Extreme PPROM complicates 0.4-0.7% of pregnancies and increases the risk of prematurity, causing a number of perinatal as well as maternal complications and increases the risk of fetal death by 1 to 2 percent.2-5
Numerous risk factors are associated with PPROM; infection (mostly bacterial infection) constitutes the major factor associated with PPROM, which activates the release of pro-inflammatory cytokines by the decidua and amniotic membranes, in which many bioactive substances like prostaglandins and metalloproteases are released. On one hand, the prostaglandins act by stimulating the contraction of the uterus; while on the other hand, the metalloproteases relax and soften the cervix, leading to membrane rupture.6 Other risk factors are thought to include race/ ethnicity. For example, Black and Hispanic women are at a higher risk in comparison to White women. Available hospital services, marital status, parity, history of preterm birth, in utero exposure to diethylstilbesterol, in vivo fertilization for index pregnancy, pregnancy complications such as gestational and pre-existing diabetes mellitus, antepartum bleeding and anemia, maternal weight gain, smoking, illegal drug use, uterine distension (e.g., polyhydramnios, multifetal pregnancy) are other factors associated with PPROM.
Sometimes PPROM can occur due to diagnostic procedures as cerclage and amniocentesis. A decrease in the collagen content of the membranes also increases the probability of membrane rupture. Maternal age may also increase the risk of PPROM, and many studies have suggested that mothers aged 30 years and above are at high risk of developing PPROM. Multiple factors are likely to predispose to such problem.7 It is especially significant if PPROM occurs prior to 26 weeks of gestation, it can lead to many maternal, fetal and neonatal complications including respiratory distress syndrome, neonatal sepsis and fetal death. The most significant maternal complication of PPROM is infection; intra-amniotic infection or chorioamnionitis is seen in 13-60% of pregnant women for example, and postpartum infection or endometritis is seen in 2-13%.
A recent study suggested that the risk of developing chorioamnionitis which poses an increased possibility of failed induction of labor resulting in cesarean section was four times higher in women with PPROM compared to women without PPROM.8 Other complications include thromboembolic disease and hemorrhage (4-12%), due to an abruption, which may be concealed.
The management of pregnant women presenting with PPROM depends on the gestational age at presentation as well as on the maternal and fetal conditions. For example, for a woman presenting before 34 weeks of gestation with PPROM but with no other maternal or fetal complications, then the conservative approach is preferred. The patient will be given antibiotics to prolong pregnancy and corticosteroids will be administered to enhance fetal lung maturity. However, there are no published studies about the risk factors, the neonatal and maternal outcomes of Oman women presenting with PPROM, especially if it occurs at an extreme gestational age. The aim of this study was therefore, to look into the associated risk factors and the maternal outcomes in Omani females presenting with extreme PPROM.
Methods
After obtaining approval from SQUH’s ethics committee, a retrospective cohort study was conducted from January 2006 to December 2011, on 44 women with PPROM before 26 weeks gestation, who delivered at SQUH and had normal fetal anatomy scan. Women with incomplete information, who ruptured membranes after 26 weeks gestation, with multiple gestations, or a preterm delivery were excluded from medical intervention and from the study. Women who delivered outside SQUH were also excluded from the study. Using the SQUH database (medical records, labor ward and neonatal intensive care unit registries), the following variables were collected; maternal demographics such as age, gravidity, parity, past obstetrical history including previous PPROM, previous surgeries, past medical history, last menstrual period, obstetric complications during the current pregnancy like gestational hypertension, gestational diabetes, antepartum and post partum hemorrhage and infection, gestational age at PPROM, gestational age at admission, steroids and antibiotics use, amniotic fluid index, gestational age at delivery, and mode of delivery. Maternal outcomes were also collected and included infection, cesarean section and antepartum hemorrhage. Gestational age was determined by last menstrual period date (if reliable), or by an obstetrical ultrasound if performed before 20 weeks gestation. Diagnosis of PPROM was based on history and vaginal examination. History of sudden discharge of amniotic fluid from the vagina or feeling wet with pooling of amniotic fluid in the posterior fornix on sterile speculum examination or a positive ferning test confirmed the diagnosis. Finally, an ultrasound was performed to determine the level of amniotic fluid index. The diagnosis of clinical chorioamnionitis was based on the presence of two or more of the following: a) the presence of purulent vaginal discharge; b) maternal pyrexia with uterine tenderness; or c) fetal tachycardia; d) clinical chorioamnionitis; or e) non-reassuring fetal heart tracing on the cardio-tocogram. Indications for delivery included clinical chorioamnionitis, fetal death and advanced labor.
An Excel sheet was used to present and analyze the data. Multivariable logistic regression was used to determine the association of baseline maternal variables (gestational age at delivery, parity, maternal age at PPROM in years and maternal BMI) and the need for caesarian section. This was done using Stata 11 (StataCorp., 2009. Stata Statistical Software: Release 11. College Station, TX: StataCorp LP). A p value of <0.05 was used for statistical significance.
Results
Forty-four women with extreme PPROM were included in this study, (Fig. 1). The mean maternal age was 30±5.4 years, (range: 18-42), while the mean gestational age at PPROM and at delivery were 20.7±3.2 weeks (range: 16-26), and 29.7±7.6 weeks (range: 17-40), respectively. Moreover, the mean parity and gravidity were 2±2.5 (range: 0-10) and 3.5±1.8 (range: 1-15), respectively. Twenty four women (55%) had infection at risk of PPROM at extreme gestational age. (Table 1)
Table 1: Maternal characteristics.
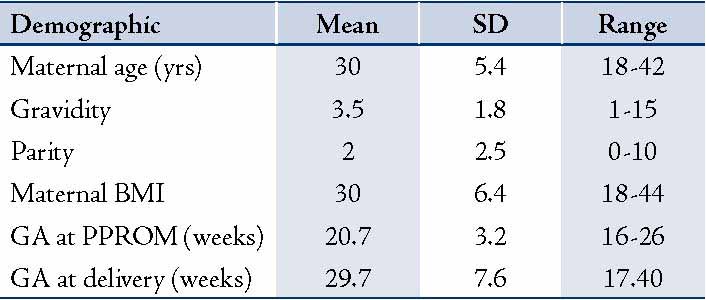
The most important risks factors associated with PPROM before 26 weeks gestation are presented in Fig. 1. The results revealed that 13 participants had a history of previous abortion and another 13 patients had chronic disease (Fig. 1). The mean BMI was found to be 30±6.4 (range: 18-44). Twenty one patients (48%) were obese, while 7 (16%) had normal BMI; and the rest (36%) were overweight. (Fig. 2)
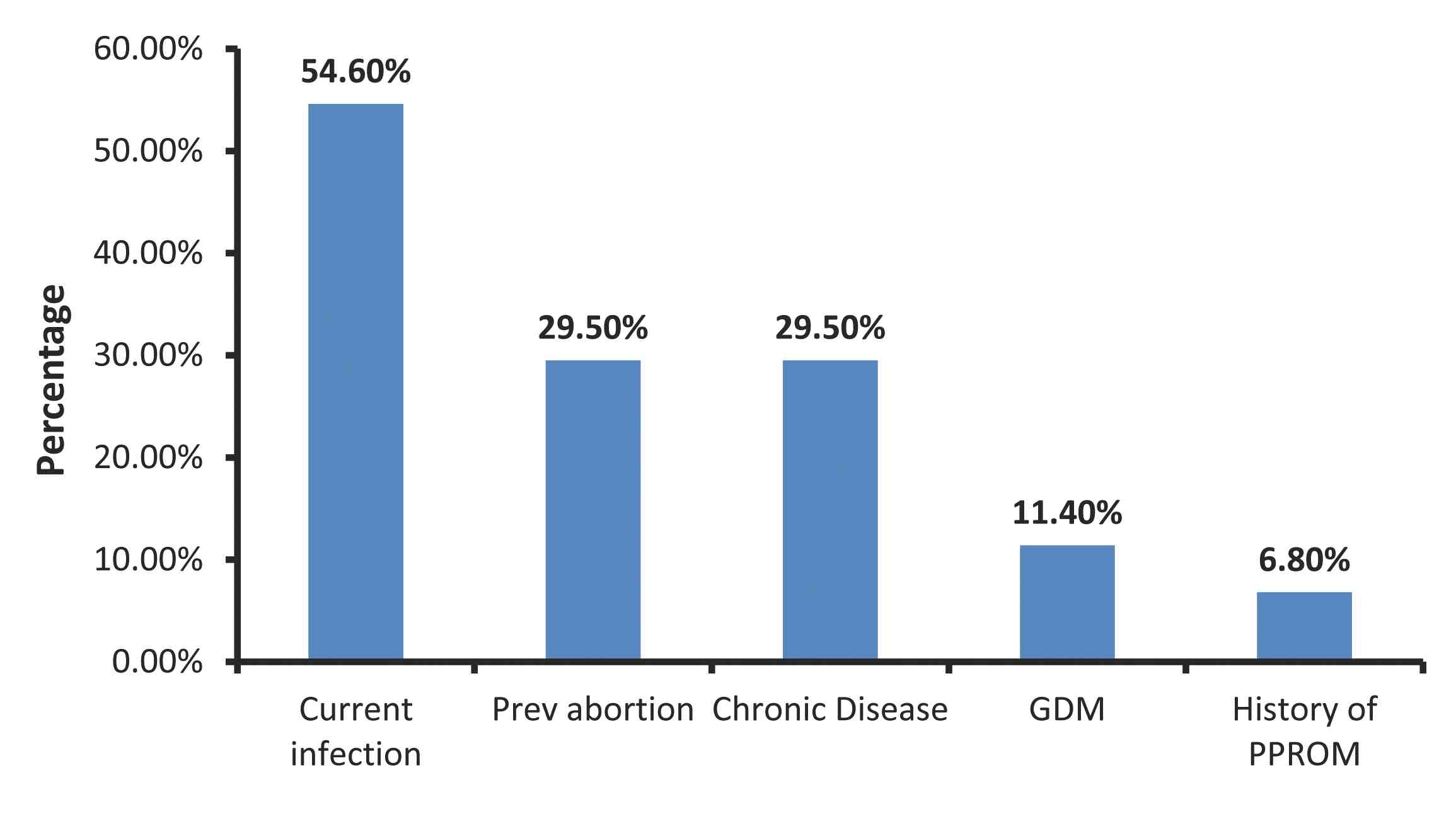
Figure 1: Maternal risk factors for extreme PPROM.
Table 2: Maternal complications.
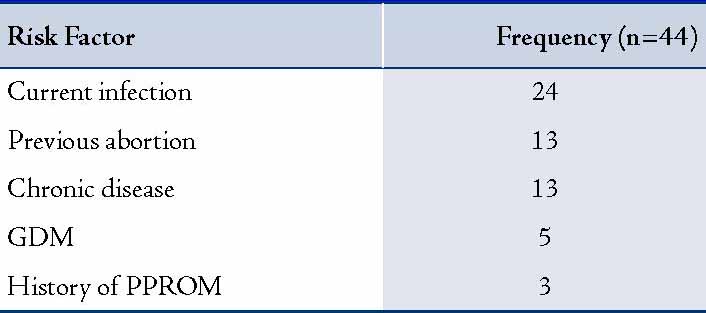
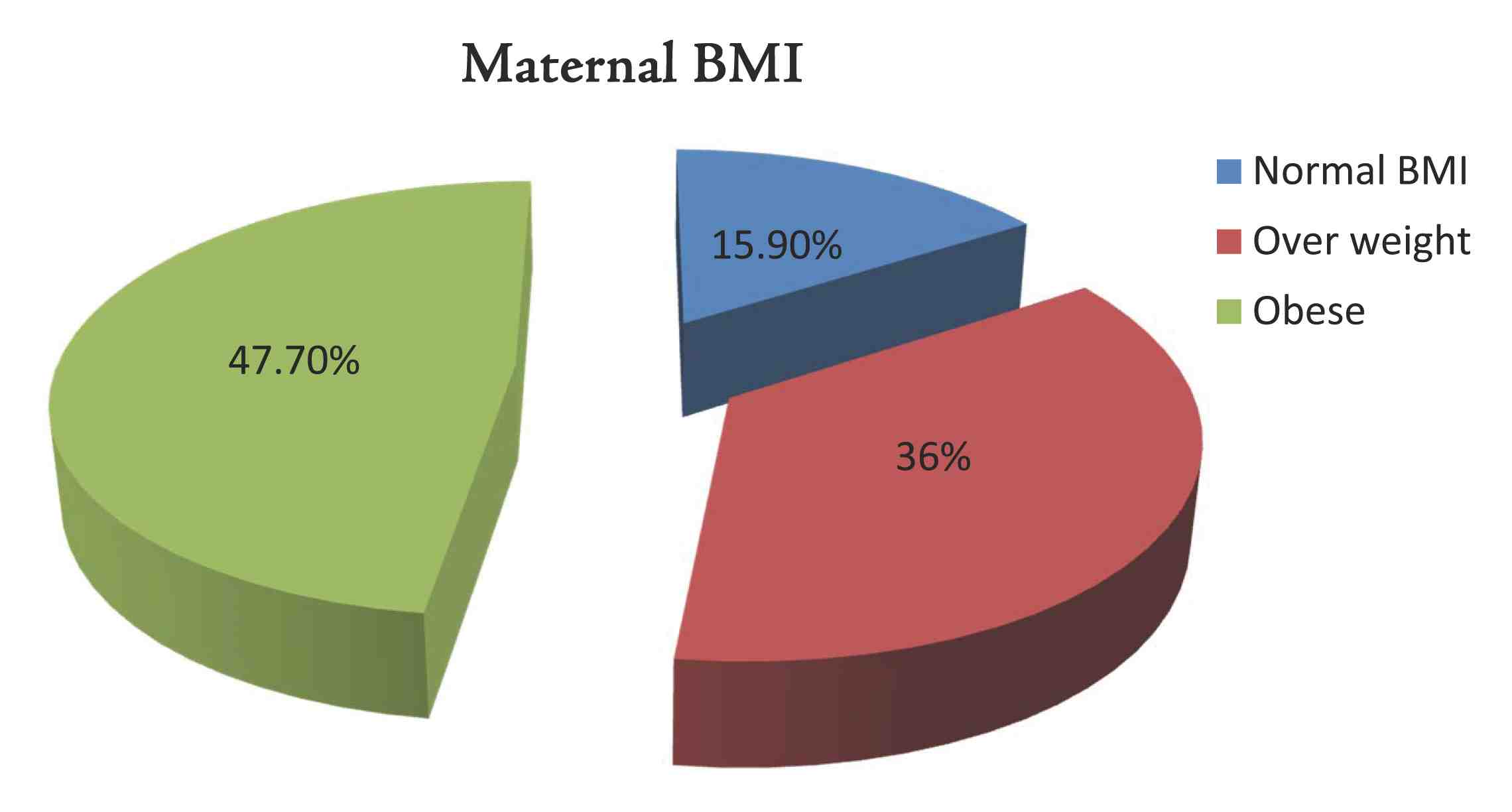
Figure 2: Maternal body mass index (BMI).
In terms of management, all patients received one course of betamethasone injection and erythromycin for 10 days. They were hospitalized with complete bed rest and were followed up for any signs of infection and fetal well-being using the biophysical profile and non-stress test. It is important to determine the latency period and its optimal length, which help to reduce the incidence of chorioamnionitis; however, there was no chance to determine it in the current study.
The study findings also revealed the most common maternal complication to be infection. Out of 44 women with PPROM, infection was observed in 20 (45%) patients, while antepartum hemorrhage was seen in 11 (25%) patients, and cesarean section was required in 12 (27%) patients. (Table 2 & Fig. 3)
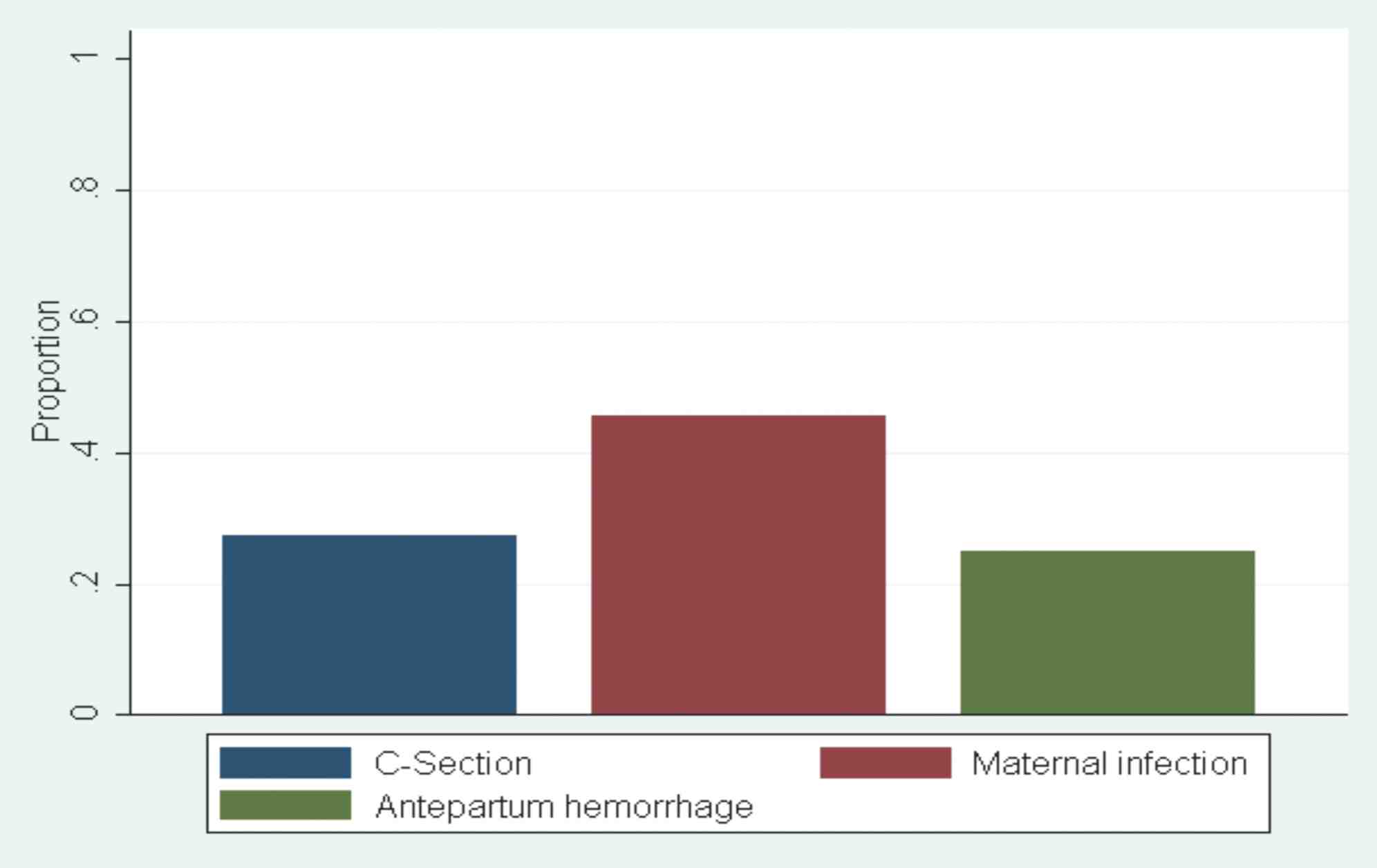
Figure 3: Maternal complications.
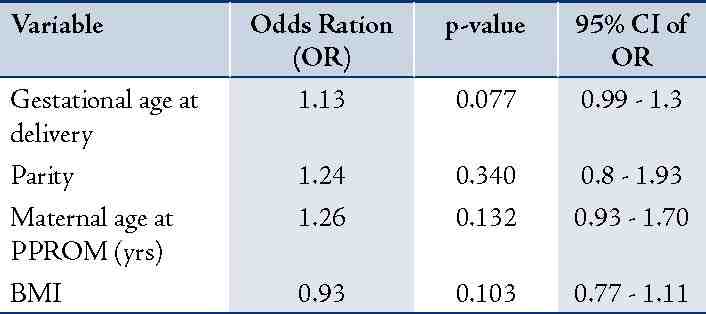
Cesarean section was the most serious and unpleasant out of the reported complications. Multivariable model (using logistic regression) was used to determine the association between baseline factors (gestational age at delivery, parity, maternal age at PPROM in years and maternal BMI) and the need for cesarean section. However, there was statistically significant association between these factors. (Table 3)
Table 3: Association between variables and cesarean section.
Discussion
The study results showed that infection, especially chorioamnionitis is frequently diagnosed in preterm delivery, which stimulate an inflammatory process that induces the preterm birth causing fetal and maternal complications. It was also noted in the current study that infection played a major role as a risk factor and was seen in 55% of the study patients. Acknowledging the major role infection plays in patients with PPROM, it is important to conduct screening of high risk patients for infection and treating them with antibiotics even prophylactically, in order to reduce the risk of PPROM in future pregnancies, especially at extreme gestational age. In addition, the findings showed that women aged 30 years and older and nulliparous women were noted to be at an increased risk of extreme PPROM. Such an association has been noted in a previous study.7
Many studies have suggested that the incidence of chorioamnionitis was approximately four times higher in patients with PPROM than in patients without PPROM. Among the most significant results in the current study was the finding that infection was implicated in 45% of patients in the postpartum period. A previous study has suggested that PPROM remained an independent risk factor associated with chorioamnionitis and that the risk of chorioamnionitis was 10 times higher for each day a preterm fetus stays in the utero with PROM.9
Intrauterine infection is known to be associated with neonatal complications such as intraventricular hemorrhage, periventricular leukomalacia, cerebral palsy, bronchopulmonary dysplasia, and neonatal death.10 Chorioamnionitis can also increase the possibility of failed induction of labor resulting in cesarean section, which was the main outcome of the complications. However, there was no significant association observed between gestational age at delivery, parity, maternal age and maternal BMI and cesarian section.
Conclusion
Infection was the most common finding in cases of extreme PPROM and it further contributed to failed induction of labor and an increase in cesarean section rates. In this study however, no association was found between the risk factors (gestational age at delivery, parity, and the maternal age at PPROM [years] and maternal BMI) and cesarean section as the outcome. This could be attributed to the small sample size and the fact that this was a retrospective study at a single tertiary center. Furthermore, the study results imply that infection plays a major role in patients with PPROM; therefore, screening of high risk women for infection and treating them with antibiotics even prophylactically might help to reduce the risk of PPROM in future pregnancies, particularly at extreme gestational age.
To our knowledge, this is the first study conducted to determine the risk factors and maternal outcomes in patients at extreme PPROM in Oman. The finding of this study should increase awareness among obstetricians on the importance of screening and monitoring patients with previous PPROM in future pregnancies, and therefore reduce maternal and fetal morbidy and mortality.
Acknowledgements
The authors reported no conflict of interest and no funding was received for this work.
References
1. Maymon E, Chaim W, Sheiner E, Mazor M. A review of randomized clinical trials of antibiotic therapy in preterm premature rupture of the membranes. Arch Gynecol Obstet 1998;261(4):173-181. .
2. Mercer BM, Arheart KL. Antimicrobial therapy in expectant management of preterm premature rupture of the membranes. Lancet 1995 Nov;346(8985):1271-1279.
3. Schucker JL, Mercer BM. Midtrimester premature rupture of the membranes. Semin Perinatol 1996 Oct;20(5):389-400.
4. ACOG Committee on Practice Bulletins-Obstetrics. ACOG Practice Bulletin No. 80: premature rupture of membranes. Clinical management guidelines for obstetrician-gynecologists. Obstet Gynecol 2007 Apr;109(4):1007-1019.
5. Waters TP, Mercer BM. The management of preterm premature rupture of the membranes near the limit of fetal viability. Am J Obstet Gynecol 2009 Sep;201(3):230-240.
6. Goldenberg RL, Hauth JC, Andrews WW. Intrauterine infection and preterm delivery. N Engl J Med 2000 May;342(20):1500-1507.
7. Berkowitz GS, Blackmore-Prince C, Lapinski RH, Savitz DA. Risk factors for preterm birth subtypes. Epidemiology 1998 May;9(3):279-285.
8. Hacker Moore Gambone. Essentials of Obstetrics and gynecology. 4th edition p: (172-179).
9. Furman B, Shoham-Vardi I, Bashiri A, Erez O, Mazor M. Clinical significance and outcome of preterm prelabor rupture of membranes: population-based study. Eur J Obstet Gynecol Reprod Biol 2000 Oct;92(2):209-216. .
10. Tanya M, Medina D, Ashley Hill. Florida Hospital Family Practice Residency Program, Orlando, Florida. Preterm Premature Rupture of Membranes: Diagnosis and Management 2006 February 15, 2006 Volume; 73(4).
|
|