Congenital thoracic aortic aneurysm (TAA) with aortic dissection is extremely rare in the pediatric population.1 About 22% of children with acute aortic dissection are reported to succumb to this catastrophic condition.2 The predisposing factors are generally genetic in origin.
Case Report
A nine-year-old girl presented with a phenotypic appearance of Noonan syndrome (NS): cleft lip and palate, low set ears, anteriorly jutting philtrum, severe club foot, cardiac lesion of large atrial septal defect (ASD), and intellectual impairment. Her NS had been genetically confirmed. At the age of two, she underwent surgical repair of a large ASD. In subsequent presentations to general practitioners, she was treated for recurrent upper respiratory tract infections. Eventually, her family discontinued medical follow-up and treated her at home using self-purchased metered-dose bronchodilator inhalers.
The patient suffered moderate respiratory distress and was presented to the local district hospital, where she was treated for acute exacerbation of bronchial asthma. She was referred to our tertiary hospital for non-invasive ventilatory support. On examination, the patient was found lethargic, hypotensive, tachypneic, and tachycardic. There was hyperdynamic pericardium and displaced apex beat. No cardiac murmur could be detected. The lungs were clear. Other systems were essentially unremarkable. Chest X-ray (CXR) showed the presence of cardiomegaly with the right heart border occupying the right hemithorax [Figure 1].
 Figure 1: Chest X-ray showing cardiomegaly with a dilated right heart border and right mediastinum.
Figure 1: Chest X-ray showing cardiomegaly with a dilated right heart border and right mediastinum.
Echocardiography revealed a moderate mitral regurgitation, with a large lesion measuring 10.3 × 8.3 cm compressed on the left ventricle, possibly of dilated ascending aorta. No thrombus or aortic regurgitation could be made out [Figure 2].
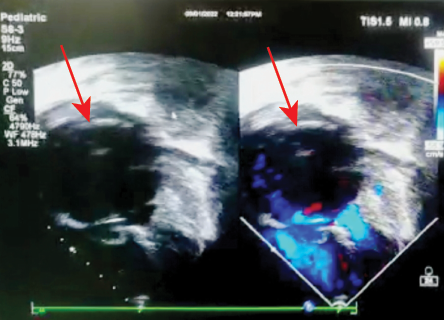 Figure 2: Short axis view of echocardiograph showing a dilated aortic root (red arrows) with blood stasis inside.
Figure 2: Short axis view of echocardiograph showing a dilated aortic root (red arrows) with blood stasis inside.
Computed tomography angiogram showed a huge aneurysm at the aortic root and ascending aorta with small dissection at the distal ascending aorta [Figures 3 and 4].
 Figure 3: Coronal and sagittal computerized tomography angiogram showing dilated aortic root and ascending aorta with small dissection (red arrow) at the distal part of ascending aorta. Aortic arch and descending aorta are seen normal.
Figure 3: Coronal and sagittal computerized tomography angiogram showing dilated aortic root and ascending aorta with small dissection (red arrow) at the distal part of ascending aorta. Aortic arch and descending aorta are seen normal.
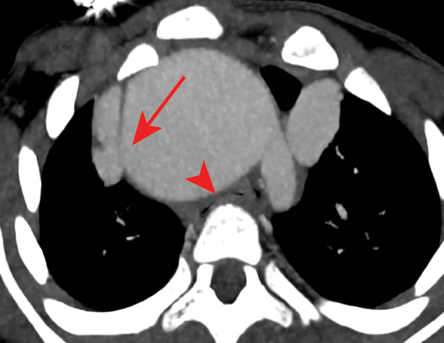 Figure 4: Axial computerized tomography angiogram showing the dissecting part of a huge ascending aorta (red arrow). Severely compressed trachea (red arrowhead) from huge aneurysm.
Figure 4: Axial computerized tomography angiogram showing the dissecting part of a huge ascending aorta (red arrow). Severely compressed trachea (red arrowhead) from huge aneurysm.
Blood parameters were normal and not suggestive of acute infections. She was subsequently intubated for worsening respiratory distress. We had difficulty ventilating her due to severe compression of the trachea because of the aneurysm [Figure 5]. The airway became severely compromised with the aneurysm of aortic root and ascending aorta, and the patient passed away.
 Figure 5: Volume rendering image of huge ascending aortic aneurysm.
Figure 5: Volume rendering image of huge ascending aortic aneurysm.
Discussion
The estimated incidence of aortic aneurysm is 5.9 cases per 100 000 persons with equal distribution in both sexes.1 Although rare, aortic aneurysm can cause mortality in children and adolescents. A retrospective study found 48 out of 128 children and youth (< 21 years) with TAA to have associated syndromes, complex congenital heart disease, or at least moderate aortic stenosis. The authors expect TAA in children and young adults to be significantly associated with genetic syndromes or cardiovascular abnormalities,2,3 as found in our patient.
TAA is mostly seen in the ascending aorta, and less frequently in the descending aorta (which occurred in the current case) and the rest of the aortic branches.4,5
NS is a genetic disorder caused by mutations altering proteins relevant to RAS/mitogen-activated protein kinase signal transduction. It is a genetically heterogeneous, pleomorphic autosomal dominant disorder6 characterized physically by hypertelorism, a downward eye slant, low-set posterior-rotated ears, short stature, short neck with webbing, cardiac anomalies, epicanthic folds, deafness, motor delay, and bleeding diathesis. Cardiac defects comprise a recognized complication. In a series of 118 patients, 27% had pulmonary stenosis or dysplasia and 25% had left ventricular hypertrophy with mostly localized septal hypertrophy with 10% having secundum ASDs. There were also reported cardiac abnormalities of ventricular septal defects, patent ductus arteriosus, tricuspid atresia, mitral stenosis, and subaortic stenosis rare reports of aortic aneurysm in NS.6 A retrospective study of echocardiograms in 37 patients with NS and without confounding medical conditions (aged 0.6 to 32 years) found that 27% had aortic annulus aneurysm while 21.6% had aortic root aneurysm.7 A few studies on individuals with NS showed a dilated aortic annulus and root were often present in childhood and very rare in adulthood, and the dilation of the aortic annulus and root can be progressive.7–9 Some NS case reports include patients who presented with aneurysms of coronary arteries,10 intracranial arteries,11 main pulmonary arteries,12 and descending aorta.13 These findings reveal that the vascular involvement in NS can be very broad.
Life-threatening forms of NS can occur in young people with congenital heart disease, connective tissue disease, or severe trauma, which call for early diagnosis and treatment.14 Aortic dissections occur in less than 3.5%, with 0.04% mortality mostly in adolescents and less commonly in children.
Aortic dissection associated with NS is exceedingly rare, with only one documented case. The patient was an adult with aortic dissection of the ascending aorta who presented with severe anterior chest pain, CXR showed widened mediastinum, and the dissection was confirmed by CTA.15
Untreated aortic dissection has a high mortality rate of 1–2% hourly for the first 48 hours from symptom onset.15 Furthermore, evaluation of predisposing factors is important, especially in cases of genetic origin, where there can also be non-cardiac causes of aortic dissection, such as connective tissue disorders. These disorders usually have clear physical stigmata associated with their own condition and autosomal dominant inheritance.16
The major presenting symptom of aortic dissection is severe anterior or posterior chest pain (in 85–95% of cases) with the first site of the pain varying and migrating to the exact site extent of the dissection.17 The CXR of aortic dissection is not always specific for aortic shadow. Patients with aortic dissection can have normal CXR, but they may have symptoms suggestive of the disease.18 However, mediastinal widening, pleural effusion, abnormal aortic contour, and cardiomegaly are the main predictors.15 Among the diagnostic radiological modalities, CTA is preferred, others being aortography, magnetic resonance imaging, and echocardiography. Transesophageal echocardiography is highly sensitive and specific for detection of intimal flap aortic dissection, and can be performed bedside in the emergency room.16
Aortic dissection is categorized into two types: type A with the involvement of the ascending aorta, and type B with restricted involvement within the aorta distal to the left subclavian artery. Our patient suffered from type A aortic dissection. Surgery is necessary for either type of dissection impending rupture, rapid progression of symptoms, or risk of malperfusion of vital organs.19 Unfortunately, surgical intervention was not possible in the current case due to the patient’s highly unstable condition and the huge aneurysm.
Conclusion
Timely identification of children or adolescents having NS with TAA complicated by airway compression may allow early medical or surgical treatment to be initiated at a younger age with possible long-term benefits and reduced mortality rates.
Disclosure
The authors declared no conflicts of interest. Written consent was obtained from the father of the patient.
Acknowledgments
We would like to thank the Director General of Health Malaysia for his permission to publish this article.
references
- 1. Bickerstaff LK, Pairolero PC, Hollier LH, Melton LJ, Van Peenen HJ, Cherry KJ, et al. Thoracic aortic aneurysms: a population-based study. Surgery 1982 Dec;92(6):1103-1108.
- 2. Joseph KC, Sameul JN. Thoracic aortic aneurysm in children their relation to rheumatic fever. Am J Dis Child 1934;48(4):780-790.
- 3. Pierpont ME, Lacro RV. Children with thoracic aortic aneurysm: challenges in diagnosis and therapy. J Pediatr 2015 Jul;167(1):14-16.
- 4. Ye C, Yin H, Lin Y, Zhou L, Ye R, Li X, et al. Abdominal aorta aneurysms in children: single-center experience of six patients. Ann Thorac Surg 2012 Jan;93(1):201-205.
- 5. Mukkannavar SB, Choudhary SK, Talwar S, Makhija N, Gulati GS, Kabra SK. Aneurysmal circumflex aortic arch. J Card Surg 2011 Sep;26(5):515-518.
- 6. Burch M, Sharland M, Shinebourne E, Smith G, Patton M, McKenna W. Cardiologic abnormalities in Noonan syndrome: phenotypic diagnosis and echocardiographic assessment of 118 patients. J Am Coll Cardiol 1993 Oct;22(4):1189-1192.
- 7. Cornwall JW, Green RS, Nielsen JC, Gelb BD. Frequency of aortic dilation in Noonan syndrome. Am J Cardiol 2014;113(2):368-371.
- 8. Morgan JM, Coupe MO, Honey M, Miller GA. Aneurysms of the sinuses of Valsalva in Noonan’s syndrome. Eur Heart J 1989 Feb;10(2):190-193.
- 9. Tartaglia M, Gelb BD, Zenker M. Noonan syndrome and clinically related disorders. Best Pract Res Clin Endocrinol Metab 2011 Feb;25(1):161-179.
- 10. Loukas M, Dabrowski M, Kantoch M, Ruzyłło W, Waltenberger J, Giannikopoulos P. A case report of Noonan’s syndrome with pulmonary valvar stenosis and coronary aneurysms. Med Sci Monit 2004 Dec;10(12):CS80-CS83.
- 11. Hara T, Sasaki T, Miyauchi H, Takakura K. Noonan phenotype associated with intracerebral hemorrhage and cerebral vascular anomalies: case report. Surg Neurol 1993 Jan;39(1):31-36.
- 12. Brown JR, Plotnick G. Pulmonary artery aneurysm as a cause for chest pain in a patient with Noonan’s syndrome: a case report. Cardiology 2008;110(4):249-251.
- 13. Paç M, Kibar AE, Oflaz MB, Paç FA. Two cases of Noonan syndrome: aortic coarctation causing a giant aneurysm of the descending aorta. Turk Kardiyol Dern Ars 2011 Oct;39(7):629.
- 14. Horwitz AE, Benz-Bohm G, Heuser L, Crespo E, Dalichau H. [Aortic dissection in childhood. Occurrence and diagnostic procedure]. Monatsschr Kinderheilkd 1986 Jan;134(1):28-31.
- 15. Shachter N, Perloff JK, Mulder DG. Aortic dissection in Noonan’s syndrome (46 XY turner). Am J Cardiol 1984 Aug;54(3):464-465.
- 16. Fikar CR, Koch S. Etiologic factors of acute aortic dissection in children and young adults. Clin Pediatr (Phila) 2000 Feb;39(2):71-80.
- 17. Rizzoli G, Scalia D, Casarotto D, Tiso E. Aortic dissection type A versus type B: a different post-surgical death hazard? Eur J Cardiothorac Surg 1997 Aug;12(2):202-208.
- 18. Hatzaras IS, Bible JE, Koullias GJ, Tranquilli M, Singh M, Elefteriades JA. Role of exertion or emotion as inciting events for acute aortic dissection. Am J Cardiol 2007 Nov;100(9):1470-1472.
- 19. Cho SH, Sung K, Park KH, Yang JH, Kim WS, Jun TG, et al. Midterm results of aortic arch replacement in a stanford type A aortic dissection with an intimal tear in the aortic arch. Korean Circ J 2009 Jul;39(7):270-274.