|
Abstract
Persistent left superior vena cava with absent right superior vena cava is a rare congenital anomaly with few cases reported to date. To the best of our knowledge, the current case is the first one to be reported from New Zealand. The condition may present difficulties in central venous catheterization, pacemaker electrode insertion and cannulation during cardiopulmonary bypass. We describe a case of persistent left superior vena cava with absent right superior vena cava, who presented with aortic stenosis (bicuspid aortic valve) and rhythm disturbances.
Keywords: Absent right superior vena cava; Persistent left superior vena cava; Vascular malformations.
Introduction
Presence of a persistent left superior vena cava (PLSVC) is considered to be one of the most frequent anomalies of the systemic venous return. In such cases, the right superior vena cava (RSVC) is generally present. However, rarely, the RSVC is absent or atretic. This malformation is often associated with other congenital heart defects. In an isolated form, the patient may be completely asymptomatic with this anomaly, and it may be accidentally detected during central venous catheterization, pacemaker electrode insertion, or at the time of cardiothoracic surgery for other conditions.
Case Report
This patient is a 69-year-old gentleman who had recently stopped smoking and was referred with clinical and echocardiographic features suggestive of severe aortic stenosis He gave a history of episodes of palpitations which were diagnosed to be supraventricular tachycardia and was treated medically.
The X-ray chest (PA view) showed bilateral emphysematous lungs, confirmed on CT scan of the chest. Pulmonary function tests were within acceptable limits (FEV1=1.82 liters; FVC=4.4 liters). He underwent an echocardiogram which showed a calcified bicuspid aortic valve with severe aortic stenosis, an aortic valve area of 0.7 cm2 and a mean gradient of 56 mmHg. All other valves were within normal limits. The right atrium and coronary sinus were found to be dilated, with no evidence of a left-to-right shunt. Coronary angiogram was essentially normal except for mild calcification in the left main coronary artery. The ascending aorta was mildly dilated with a diameter of 40 mm.
He was taken up for an aortic valve replacement. There was difficulty encountered during central venous cannulation through the right internal jugular vein as the catheter could not be advanced beyond a certain length; however, since the central venous pressure trace was showing an acceptable graph, the catheter was fixed at the 12 cm mark. During the surgery, the right atrium was found to be dilated. The innominate vein was situated in a higher than usual position. RSVC was found to be absent and represented by a fibrous strand without any lumen and a large PLSVC was found draining into the coronary sinus, (Figs. 1 and 2). There was no other congenital cardiac anomaly noted. Only antegrade blood cardioplegia was used. The routine retrograde cardioplegia could not be used as the coronary sinus was hugely dilated due to PLSVC draining directly into it.
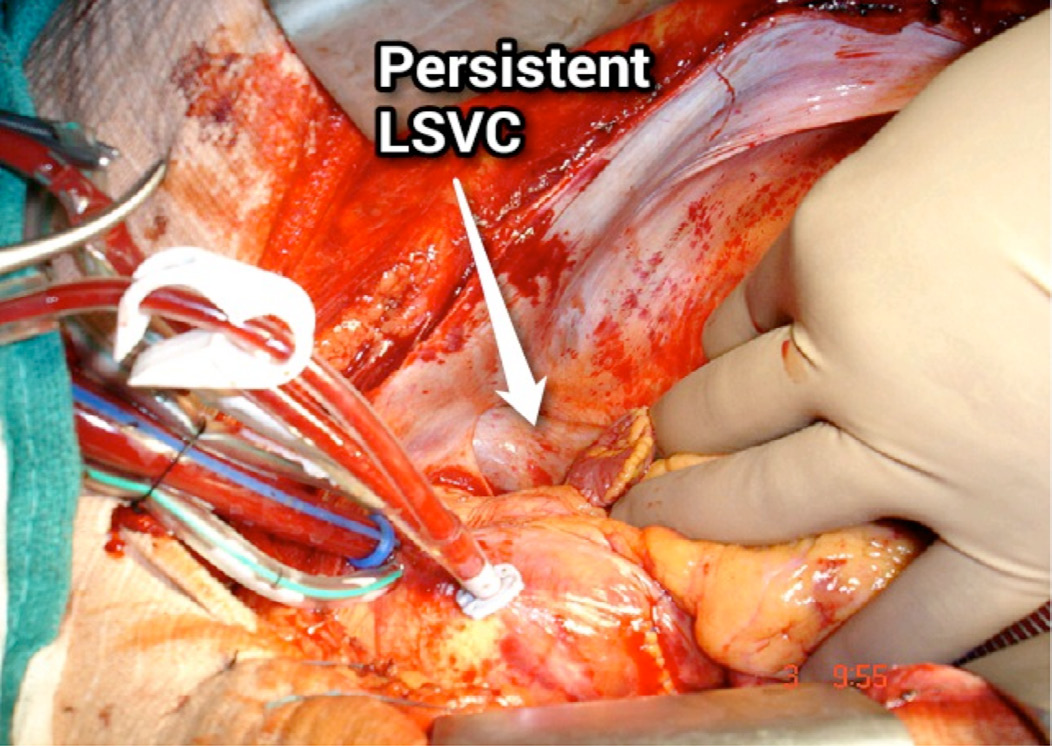
Figure 1: Operative picture showing PLSVC.
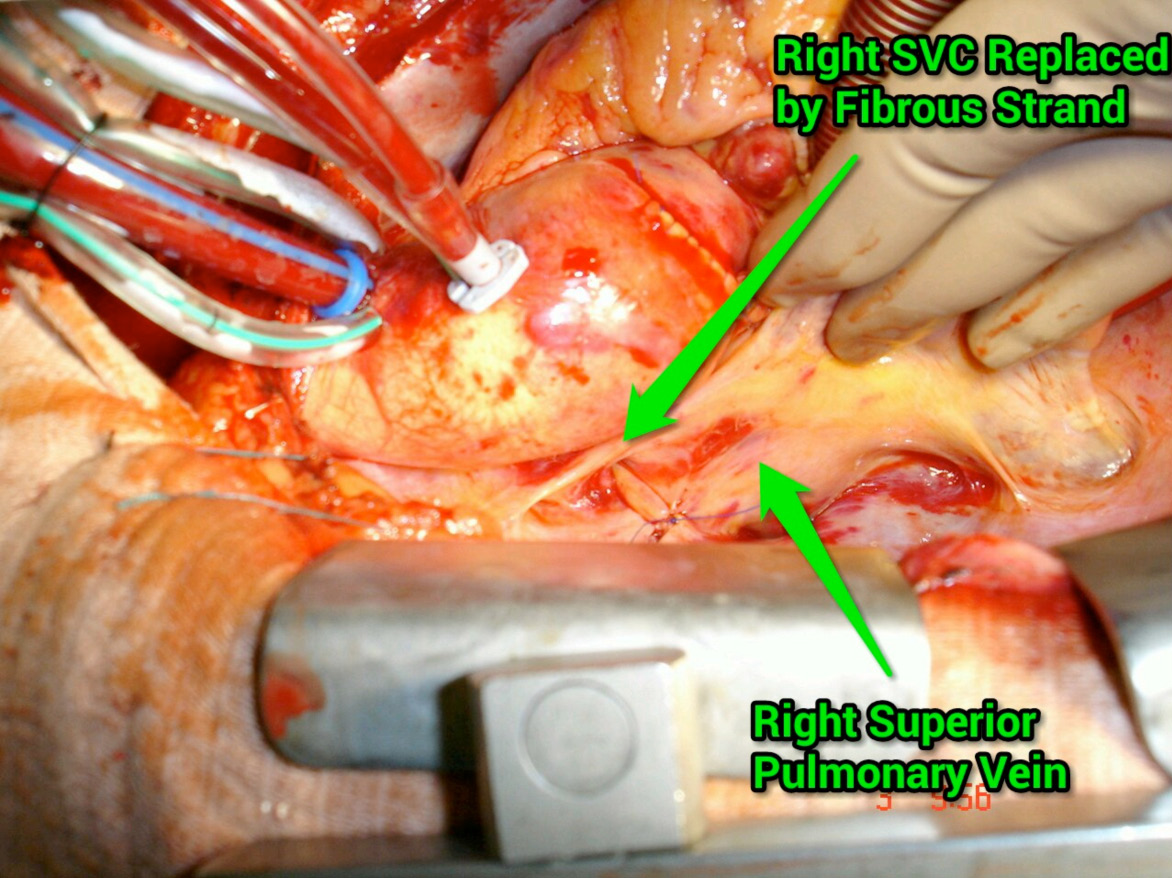
Figure 2: Operative picture showing RSVC replaced with fibrous strand
The aortic valve was bicuspid and heavily calcified. It was excised and replaced with a 25 mm St. Jude bileaflet mechanical aortic valve after decalcification of the annulus. He made an uneventful recovery and was discharged on the 7th postoperative day on warfarin. Retrospectively, the investigations were reviewed. Chest X-ray showed a vertical structure in the left mediastinum which was most likely the PLSVC. The CT scan of the chest confirmed the presence of PLSVC and an atretic RSVC, (Figs. 3 and 4). The echocardiogram also showed presence of PLSVC, but whether or not the RSVC was present was not clear.
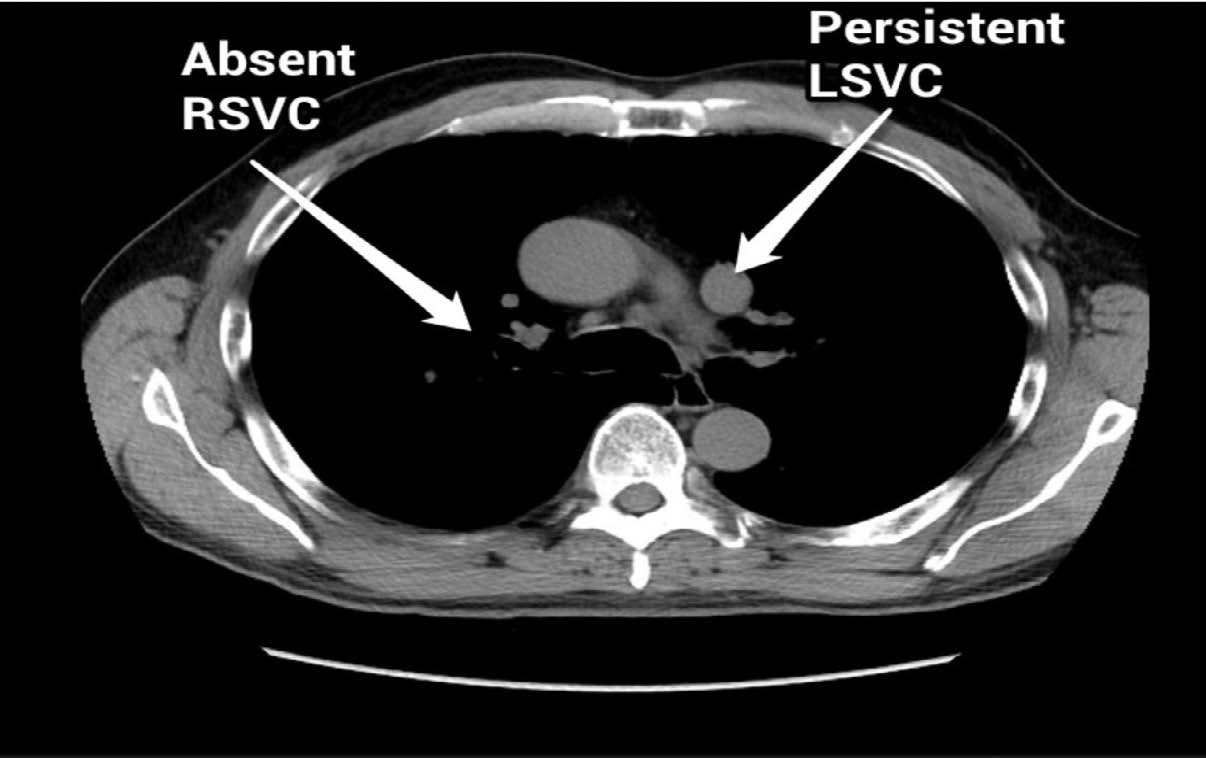
Figure 3: Coronal section of CT scan showing PLSVC and atretic RSVC.
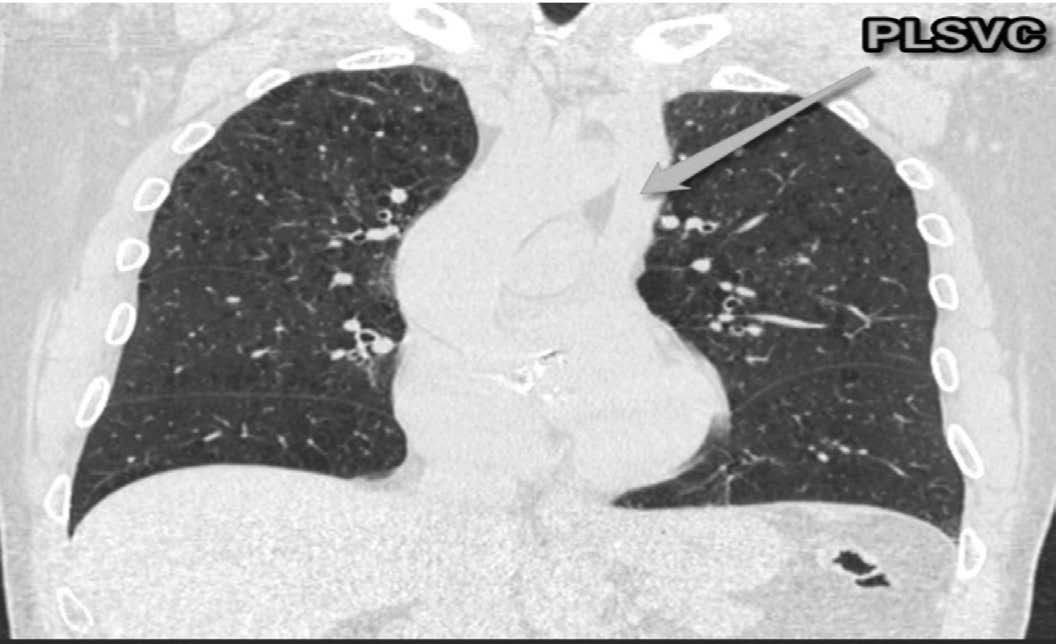
Figure 4: PLSVC on reconstructed CT scan image.
The diagnosis was thus made intraoperatively and had been completely missed on all the preoperative investigations. This was possibly because it is a very rare anomaly and it was not suspected and not specifically looked for. However, this anomaly can cause several intraoperative and postoperative problems. Therefore, it is recommended that the clinicians should actively look for this anomaly during the preoperative evaluation of a patient especially in the presence of a dilated coronary sinus of more than 1 cm in diameter.
Discussion
The presence of left superior vena cava (LSVC) occurs in approximately 0.3% to 0.5% of the general population.1,2 Its incidence is ten-fold higher in patients with congenital heart malformation.2,3 PLSVC with absent RSVC occurs in only 0.09% to 0.13% of patients with congenital heart defects.4 It is a rare anomaly with only a handful of cases reported to date. The first case of PLSVC with absent RSVC was reported in 1862.5 To the best of our knowledge, this is probably the first case of absent RSVC, PLSVC with congenitally bicuspid aortic valve, being reported from New Zealand. Whether or not this association of congenitally bicuspid aortic valve with absent RSVC and PLSVC is statistically significant will only come to light once more cases of this rare entity are reported from different parts of the world.
During fetal development, failure of closure of the left anterior cardinal vein results in PLSVC. Most of the times, it drains into the coronary sinus, but if the developmental arrest occurs at an earlier stage, then PLSVC may drain into the left atrium directly or through an unroofed coronary sinus.6 In a review of 121 cases of PLSVC with absent RSVC by Bartram et al, 46% of the cases were associated with additional cardiac anomalies.7 Most common congenital defects associated with combined great venous malformation were various types of atrial septal defects, endocardial cushion defects, and tetralogy of Fallot. Other reported co-existent congenital anomalies were coarctation of aorta, ventricular septal defect, double aortic arch, and transposition of great arteries, dextrocardia, and asplenia.
An absent RSVC can lead to inability to insert central venous canula, pulmonary artery catheter, and transvenous pacing leads through right internal jugular or subclavian vein.8 In addition, a persistent LSVC may lead to several clinical issues which include the following:8
1. Difficulty inserting central venous cannula, pulmonary artery catheter, and transvenous pacing leads through left internal jugular/subclavian vein. The dilated coronary sinus which is thin walled and stretched predisposes it to perforation, tamponade, various arrhythmias, and cardiac arrest.
2. PLSVC may require separate cannulation during right-sided open-heart surgical procedures, either directly or through the coronary sinus (CS).
3. Difficulty in performing cavo-pulmonary anastomoses.
4. Inability to deliver retrograde cardioplegia during open-heart surgery and port-access cardiac surgery because of large size of coronary sinus.
5. Rhythm abnormalities such as ectopic atrial rhythm, wandering pacemaker, first-degree atrioventricular block, tachyarrhythmia, and complete heart block because of stretching or fragmentation of the atrioventricular node and His bundle secondary to dilatation of coronary sinus. Sinoatrial nodal abnormalities have been detected in patients with absent RSVC, predisposing the patient to sick sinus syndrome.9
6. Rarely, enlarged CS can impinge on the vestibule of the mitral valve that may produce obstruction to left ventricular inflow.
7. Orthotopic heart transplant may require the recipient’s heart to be excised along the atrioventricular grove, preserving the persistent left superior vena cava and coronary sinus.
In view of the above-mentioned anticipated intraoperative implications, it is advisable to investigate a dilated coronary sinus (CS) more than 1 cm in diameter thoroughly. The enlargement of the CS may indicate right atrial hypertension, an anomalous systemic venous channel, fistulous communication with coronary arteries, and total or partial anomalous pulmonary venous drainage.8
The available diagnostic modalities for the diagnosis of this relatively rare anomaly are as follows:10
1. Echocardiogram: Transthoracic or transesophageal. The transesophageal echocardiogram is more sensitive for the diagnosis and also detects other associated anomalies.
2. Injecting agitated saline as a contrast in the left antecubital vein during the echocardiogram appears first in the persistent LSVC, coronary sinus, and right atrium in that order. In case of an absent or atretic RSVC, similar injection into the right antecubital vein also appears first in the coronary sinus, as the blood flows through the right brachiocephalic vein into the LSVC and then to the coronary sinus.
3. Contrast upper venous digital subtraction cavography is the diagnostic modality for confirmation of PLSVC with or without associated absent/atretic RSVC.
4. CT and MRI are now picking up as important aids in the diagnosis of this anomaly.
Conclusion
Atretic or absent RSVC with a PLSVC is a very uncommon congenital anomaly. This anomaly has several clinical and operative implications. A preoperative diagnosis with the aid of current imaging modalities is imperative to anticipate and avoid any complications. The radiologists, sonographers, intensivists, interventionists, and cardiothoracic surgeons should be aware of the existence of this anomaly and should look for specific features at the slightest indication of its existence.
References
1. Chandra A, Reul GJ Jr. Persistent left superior vena cava discovered during placement of central venous catheter. Tex Heart Inst J 1998;25(1):90.
2. Wood PH. Diseases of the heart and circulation 2nd edition. Philadelphia: JB Lippincott 1956; 457.
3. Zellers TM, Hagler DJ, Julsrud PR. Accuracy of two-dimensional echocardiography in diagnosing left superior vena cava. J Am Soc Echocardiogr 1989 Mar-Apr;2(2):132-138.
4. Camm AJ, Dymond D, Spurrell RA. Sinus node dysfunction associated with absence of right superior vena cava. Br Heart J 1979 Apr;41(4):504-507.
5. Halbertsma MJ. Abnormalitaet der vena cava superior. Nederl Tijschr Geneesk. 1862;6:610-612.
6. Fischer DR, Zuberbuhler JR. Anomalous systemic venous return. In: Anderson RH, Baker E, Mccartney RF, eds. Paediatric Cardiology. New York: Churchill Livingstone, 2002; 851-65.
7. Bartram U, Van Praagh S, Levine JC, Hines M, Bensky AS, Van Praagh R. Absent right superior vena cava in visceroatrial situs solitus. Am J Cardiol 1997 Jul;80(2):175-183.
8. Neema PK, Manikandan S, Rathod RC. Absent right superior vena cava and persistent left superior vena cava: the perioperative implications. Anesth Analg 2007 Jul;105(1):40-42.
9. Lenox CC, Hashida Y, Anderson RH, Hubbard JD. Conduction tissue anomalies in absence of the right superior caval vein. Int J Cardiol 1985 Jul;8(3):251-260.
10. Pálinkás A, Nagy E, Forster T, Morvai Z, Nagy E, Varga A. A case of absent right and persistent left superior vena cava. Cardiovasc Ultrasound 2006;4:6.
|