|
Abstract
Objective: To assess the usefulness of a computed tomography scan in patients with non-localized headache.
Methods: One-hundred and forty-two patients with non-localized headache were included in a retrospective study after reviewing the medical records of 896 patients at the Radiology Department, Sultan Qaboos University Hospital. Patients with neurological deficits, head injury, previous intracranial intervention, or malignancy were excluded. Radiological findings of all patients were reviewed and results were divided into 3 groups: 1) no intracranial abnormality; 2) with clinically significant intracranial abnormality; and 3) positive without clinical significance or with extracranial abnormality. All patient history records were reviewed for a period of six months following their initial computed tomography scan to assess their clinical outcomes. The cost of computed tomography examination and patient radiation dose were calculated.
Results: Of the 142 patients, 64% were females and 36% males (7% pediatric) with an age range of 4-87 years (mean: 36.2 years). Among the patients, 70% demonstrated negative computed tomography findings (grade 1), only 4% showed clinically significant findings (grade 2), and 26% demonstrated incidental positive findings with no clinical significance (grade 3). The average cost of computed tomography head examination was approximately 60 Omani Riyal ($156). The clinically significant positive cases were fewer than expected. The average estimated radiation dose for these patients was calculated and found to be around 5 times the radiation from computed tomography of the sinuses (approximately 1.84 mSv).
Conclusion: Computed tomography head imaging in patients with non-localized headache has a low likelihood for any significant intracranial lesion. Therefore, it is essential to develop local standard operating procedures to promote better utilization of this type of imaging service.
Keywords: Computed tomography; CT head; Non-localized headache; Non-focal headache.
Introduction
Headache or cephalalgia is defined as diffuse pain not confined to the area of distribution of a nerve.1 It is one of the most common disorders experienced by patients which results in a visit to a physician. This is the most common symptom for which patients are referred by the physicians. It has been shown that 95% of young women and 91% of young men experienced headache during a 12-month period, and of these, 18% of women and 15% of men consulted a physician.2 Generally, 46% of the adult population experiences a headache disorder, while 11% suffer from migraine headache and 42% from tension-type headache. Approximately 3% experience chronic daily headache.3,4
Most patients presenting with the sole symptom of headache with no focal neurological deficits can be managed without radiological imaging. However, with the expansion of imaging centers, increasing patient demand for thorough and "high-tech" evaluation and the increasing practice of "defensive medicine," neuroimaging -in the form of CT or MRI- is widely used to evaluate headache.2,5-7 Headache also continues to account for a large number of visits to the emergency department.5 However, a large proportion of the imaging studies in these patients are negative.6,7 Due to these factors, this study was done to examine the diagnostic outcomes of CT imaging in patients presenting with non-localized headache at Sultan Qaboos University Hospital (SQUH).
Methods
A retrospective analysis of all CT head requests at SQUH during the period of 1st May 2009 to 31st October 2009 was performed. Patients with non-localized headache were included and those with neurological findings, history of head injury, previous intracranial intervention or malignancy, which by itself would warrant a CT head, were excluded.
One-hundred and forty-two of 896 CT head examinations performed at SQUH during this period satisfied the inclusion criteria. Clinical and radiological findings of all of these patients were reviewed. The standard protocol of plain CT scan head was adopted and was performed with the patient in supine position. Sequential 5 mm scans were obtained from the angle of the mandible to the vertex of the skull using a Siemens Somatom Sensation scanner using the standard head CT protocol (120 kV, 380 mAs for adults and 120 kV 190 mAs for pediatric patients). This study was approved by the institutional research committee which authorized the review of the patients' charts.
CT images were reviewed by an experienced radiologist and the results were divided into three groups: 1) no intracranial abnormality (negative study); 2) clinically significant intracranial abnormality, such as space-occupying lesions or intracranial hemorrhage (Table 1); and 3) positive without clinical significance or with extracranial abnormality (e.g., sinusitis, ischemic or atrophic changes or incidental findings which do not explain the headache). This was a similar approach to that used in the previous studies assessing MRI and CT scan use in management of non-focal headache.5,6 Follow-up clinical notes of all these patients were reviewed for six months after the initial CT examination to assess the outcome and impact on management.
The average estimated radiation dose for CT head of these patients was calculated (Dose-Length Product; DLP: 800 mGy/cm, effective dose: 1.84 mSv) and for CT sinuses (DLP: 140 mGy/cm, effective dose: 0.32 mSv). The average DLP was obtained from the patients' imaging protocol and then the effective dose was calculated by multiplying the DLP (in Gy/cm) by the factor 0.0023 mSv mGy-1 cm-1 to obtain an effective dose in mSv for the patients.9 Hence, the radiation dose for the patient from CT head was approximately 5 times the radiation from CT sinuses. The cost of each CT head study was around 60 OR ($156) and for MRI brain was 100 OR ($260).
Results
One-hundred and forty-two out of 896 (16%) patient records satisfied the inclusion criteria. The patients were between 4 to 87 years of age (mean age: 36.2 years). Of these, 64% were females, 36% were males (F:M ratio = 1.8:1), wherein 7% (n=10) were pediatric patients (<13 years), (Fig. 1). Also, the scans of 100 (70%) patients showed negative CT findings and they were categorized as grade 1, while 42 (30%) patients showed positive CT findings which were classified as grade 2 or grade 3. In grade 1, there was a female sex predominance (F:M ratio=2:1) which may be explained by the larger female number in the studied group. In grade 2 category of the positive results, 6 (4%) patients showed clinically significant findings which impacted on patient management (mean age: 40.2 years), (Table 1, Fig. 2). There were 36 (26%) patients with grade 3 positive scans (F: M=2.7:1) which included old infarcts, chronic small-vessel ischemic changes, encephalomalacia and extracranial abnormality like sinus opacification or mucosal thickening. In this group, 7% of the patients had sinus-related headache (Fig. 3). The majority of normal CT findings were associated with younger age (mean: 32.2 years) compared to cases with identifiable cranial abnormalities (mean age: 47.7 years). This category also included all the pediatric cases.
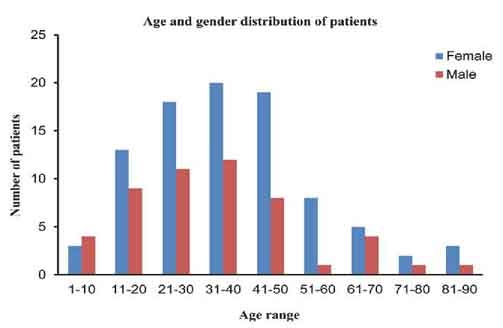
Figure 1: Age and gender distribution of the studied group of patients. It shows that most of the cases presented to the hospital with non-localizing headache during the study period were young female patients.
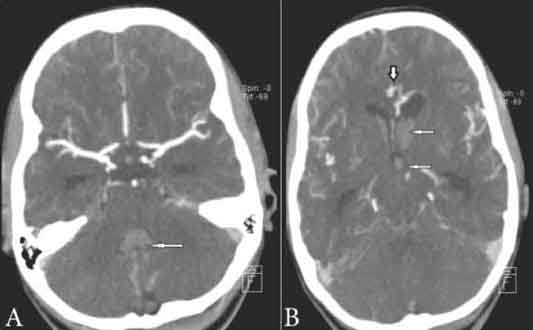
Figures 2a & 2b: CT brain post IV contrast. There was extensive hemorrhage noted in the frontal horns of the lateral ventricles, third ventricle and fourth ventricle (thin arrows) with associated ventriculomegaly. There was hemorrhage in the cisterna magna with effacement of the sulci. A small arteriovenous malformation was noted with a 1.5 cm nidus (thick arrow) anterior to the frontal horns of the lateral ventricle at the midline. The remainder of the vascular structures appear within normal.
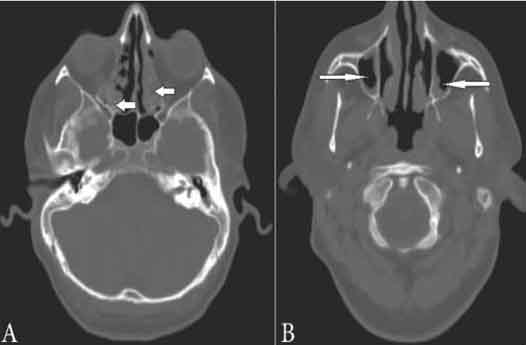
Figures 3a & 3b: Plain CT scan of head (CT sinuses). Normal brain scan showed mucosal thickening in the maxillary (thin arrows) and ethmoid (thick arrows) sinuses. Small polypoidal thickening in the right sphenoid sinus. No evidence of fracture.
In addition, 4 out of 42 patients with suspicious findings on CT head led to further examination with brain MRI which showed no abnormality. Four adult patients died, three of them had negative CT head and died of other causes (aspiration pneumonia, sepsis, and hepatic encephalopathy with gallbladder cancer). One of them died due to pontine hemorrhage which was detected on CT head. Moreover, 20 out of the 142 (20%) patients were followed-up at the psychiatric clinic for various psychiatric illnesses. Most of these patients (n = 17) had negative findings on CT head (Category 1) and only 3 patients had category 2 findings (incidental falx lipoma, age related brain atrophy and sinusitis).
Discussion
The results of the present study match similar studies conducted by Jordan YJ et al. which, however, studied "patients who only presented to the emergency department with non-focal headache" and "the economic impact and utility of MRI in patients with non-focal headache." The same categorization system in that study was used to classify the participants in the current study into 3 groups.5,6 The female patients in this study were double the number of the male patients and most of them were aged between 20 to 50 years which is regarded as a young age group and the majority of the patients were classified as category 1.
It is interesting to note that in the current work, a somewhat higher percentage (4) of clinically significant cases (subarachnoid and intracerebral hemorrhage, Pontine hemorrhage, arachnoid cyst, cerebritis, brain tumor, malignant otitis externa with osteomylitis of the skull bone) were found than those observed by other authors. Most have shown less than 2% of patients presenting with non-focal headache.6,9,10 Jordan YJ et al. and Jordan et al. demonstrated 1.02% and 1.5%, respectively, of clinically significant results that required a change in management.5,6 The present findings indicate that the utility of CT scan in patients with non-focal headache has low positive yield which concurs with prior studies that found CT scan to have limited utility in this group of patients.5,6,10-13
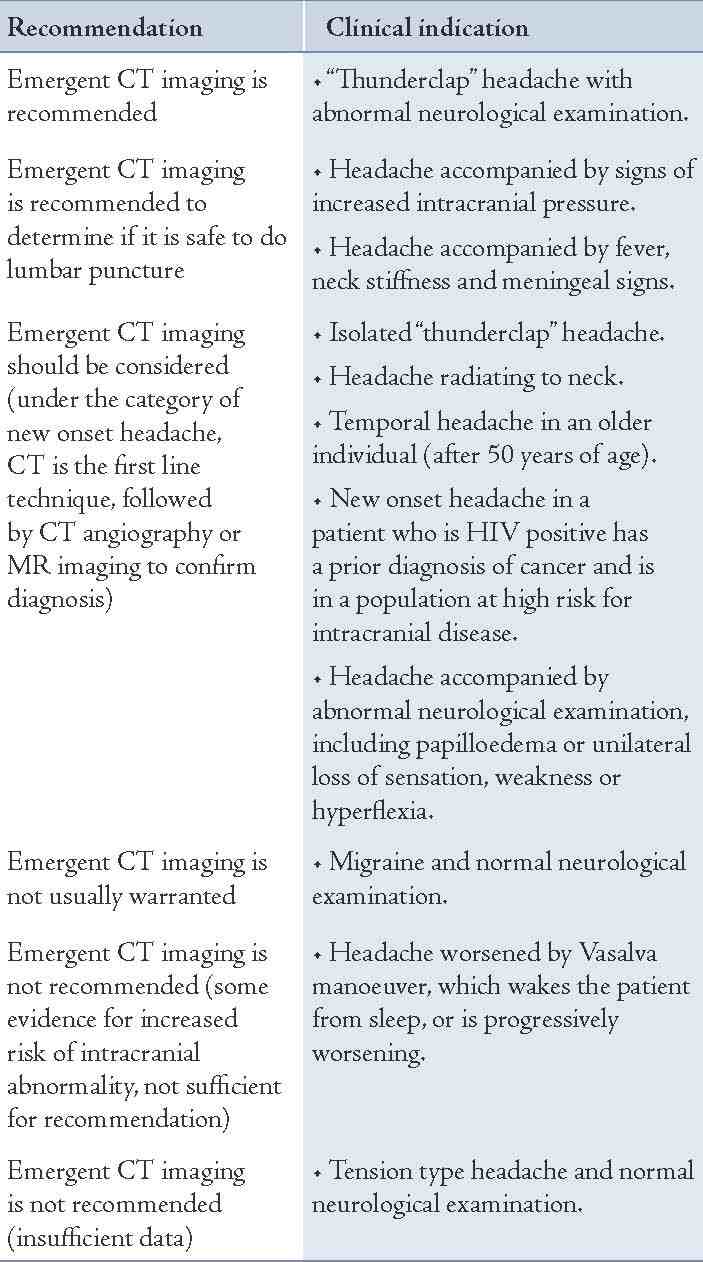
Guidelines have been developed for imaging headache by the American College of Emergency Physicians, and the American College of Radiology Expert Panel on Neuroimaging.3,14 The consortium's guidelines are based on extensive peer-reviewed literature and the accumulated evidence. The general recommendations suggest that screening patients with isolated headache by CT or MRI is usually not warranted and neuroimaging should be considered in patients with non-acute headache and unexplained abnormal findings on neurologic examination (Grade B recommendation). Patients with a history of cancer or those who are in high-risk groups for intracranial diseases are also more likely to have pathology detected at imaging and should be imaged.3,5,14 In line with these guidelines, local standard operating protocols should be developed for patients with non-localized headache. This will enable the radiologist to prioritize the requests, thus reducing the waiting time and reducing the demand on the radiology department. The guidelines are summarized in Table 1.
Table 1: Guidelines* for neuroimaging (CT) in patients with headache.
Previous studies have shown that CT and MRI imaging of non-focal headaches yield a low percentage of positive clinically significant results.9,15,16 It is estimated that CT scan accounts for 10% of all diagnostic radiological examinations and contributes up to 70% of the collective radiation dose delivered to patients.17 The growing use of CT scan is accompanied by the growing concerns about risks associated with radiation exposure. The National Academy of Science has published a series of reports about the biological effects of ionizing radiation. It estimated that a single dose of 10 mSv is associated with a lifetime risk of 1:1000 for developing solid cancer or leukemia.9,18 Thus the benefit to risk ratio for any patient will be driven by the benefit and appropriateness of CT examination. In this study, 7% of the patients could have had less radiation dose by undergoing proper CT scan such as CT sinuses. If the correct examination was requested by the physician and proper history was provided in the request form, undue radiation exposure could have been avoided. In addition, the average cost to perform a CT head at SQUH was 60 OR ($156). Hence, the total cost for the total studied population was 8,520 OR ($22,200) excluding the additional cost incurred for those who then underwent brain MRI, which also showed negative results (400 OR; $1,000). Since only 4% of the studied patients' imaging were significantly positive, then the total cost per clinically significant CT findings detected was 240 OR ($600).
Although 14% of the patients with negative CT scans were then followed-up at the psychiatric clinic, it is not clear how significantly the CT scan findings had aided the management of these patients. Setting up standard operating procedures (SOPs) and developing pathways for the clinicians to refer such patients will definitely improve the quality of care and will undoubtedly reduce the patients' exposure to radiation as well as the overall cost on the radiology deparment, and thus improve the radiology services by minimizing long waiting lists which remains a priority given the growing demands on the radiology department.
Conclusion
CT head imaging in patients presented with non-localizing headache yields a low percentage of clinically significant positive results. Therefore, a local clinical practice guideline seems necessary for decision making with respect to imaging. This will aid towards prioritizing high risk patients and will act as a guide towards the appropriate imaging modality. It will certainly reduce unnecessary radiation exposure to patients as well as reduce the waiting time for imaging services provided by the radiology department.
Acknowledgements
The authors reported no conflict of interest and no funding was received for this work.
References
1. Randall C, Edward FH. Evaluation of Acute Headache in Adults. Amer Fam Phys. 2001;63(4):685-692.
2. Parizel PM, Voormolen M, Van Goethem JW, van den Hauwe L. Headache: when is neuroimaging needed? JBR-BTR 2007 Jul-Aug;90(4):268-271.
3. Stovner Lj, Hagen K, Jensen R, Katsarava Z, Lipton R, Scher A, et al. The global burden of headache: a documentation of headache prevalence and disability worldwide. Cephalalgia 2007 Mar;27(3):193-210.
4. Al-Shimmery EK. Precipitating and relieving factors of migraine headache in 200 iraqi kurdish patients. Oman Med J 2010 Jul;25(3):212-217.
5. Jordan YJ, Lightfoote JB, Jordan JE. Computed tomography imaging in the management of headache in the emergency department: cost efficacy and policy implications. J Natl Med Assoc 2009 Apr;101(4):331-335.
6. Jordan JE, Ramirez GF, Bradley WG, Chen DY, Lightfoote JB, Song A. Economic and outcomes assessment of magnetic resonance imaging in the evaluation of headache. J Natl Med Assoc 2000 Dec;92(12):573-578.
7. Alehan FK. Value of neuroimaging in the evaluation of neurologically normal children with recurrent headache. J Child Neurol 2002 Nov;17(11):807-809.
8. Huda W, Ogden KM, Khorasani MR. Converting dose-length product to effective dose at CT. Radiology 2008 Sep;248(3):995-1003.
9. Sun Z, Ng KH, Vijayananthan A. Is utilisation of computed tomography justified in clinical practice? Part I: application in the emergency department. Singapore Med J 2010 Mar;51(3):200-206.
10. Akpek S, Arac M, Atilla S, Onal B, Yücel C, Isik S. Cost-effectiveness of computed tomography in the evaluation of patients with headache. Headache 1995 Apr;35(4):228-230.
11. Noor UI, Ayesha A, Kalsoom N. Cranial Computed Tomgraphy in Patients with Headache. J Med Sci 2009;17(1):19-21.
12. Olesen J. The classification and diagnosis of headache disorders. Neurol Clin 1990 Nov;8(4):793-799.
13. Prager JM, Mikulis DJ. The radiology of headache. Med Clin North Am 1991 May;75(3):525-544.
14. Benjamin M, Jay H, David B, Douglas C, Michael P, Todd D, et al. Evidence-based Guidelines in the Primary Care setting: Neuroimaging in Patients with Nonacute Headache. Am Fam Physician 2005 Mar;71(6):1219-1222.
15. Grosskreutz SR, Osborn RE, Sanchez RM. Computed tomography of the brain in the evaluation of the headache patient. Mil Med 1991 Mar;156(3):137-140.
16. Veingarten S, Kleinman M, Elperin L, Larson EB. The effectiveness of Cerebral Imaging in the Diagnosis of Chronic Headache. Arch Intern Med 1992;152(12):1457-1462.
17. Fazel R, Krumholz HM, Wang Y, Ross JS, Chen J, Ting HH, et al. Exposure to low-dose ionizing radiation from medical imaging procedures. N Engl J Med 2009 Aug;361(9):849-857.
18. Committee to Access Health Risks from Exposure to Low Level of ionizing Rdiation, National Research Council. Health risks from Exposure to low level of ionizing radiation, BEIR VII Phase2. Washington: National Academies Press, 2006.
|