| |
Abstract
Objective: To compare the efficacy of behavioral intervention program and vaginal cones on stress urinary incontinence.
Methods: In this randomized clinical trial, 60 women aged 25-65 years with stress urinary incontinence were randomly divided into two groups, those who participated in a behavioral intervention program (n=30) and those who used vaginal cones (n=30). The women in the behavioral intervention group were instructed on pelvic floor exercise and bladder control strategies. In the other group, pelvic floor exercises were performed using the vaginal cones. All participants were treated for 12 weeks and followed-up every 2 weeks. The subjective changes in severity of stress urinary incontinence were measured using a detection stress urinary incontinence severity questionnaire, leakage index, and a 3-day urinary diary. The objective changes were measured by pad test. For better evaluation of the effects, two questionnaires were used: Incontinence Quality of Life and King’s Health Questionnaire.
Results: Among the 51 women who completed the study, 25 subjects were in the vaginal cones group and 26 participated in the behavioral intervention program. The changes in leakage rate on pad test and leakage index in the behavioral intervention program group were significantly higher than in the vaginal cones group (p=0.001 and p=0.008, respectively), but the severity of stress urinary incontinence was not significantly different between the two groups (p=0.2). The changes in strength of the pelvic floor, Incontinence Quality of Life, and King’s Health Questionnaire scores showed no significant differences between the two groups after 12 weeks of intervention.
Conclusion: Vaginal cones and behavioral intervention programs are both effective methods of treatment for mild to moderate stress urinary incontinence, but the behavioral intervention program is superior to vaginal cones in terms of cost-effectiveness and side effects.
Keywords: Behavioral intervention program; Vaginal cones; Stress urinary incontinence.
Introduction
The most common type of urinary incontinence (UI) in women is stress incontinence that is defined as the involuntary loss of urine during coughing, sneezing or physical exertion such as sporting activities or sudden change in position. It produces serious economic, social and psychological problems with loss of self-confidence, feelings of helplessness, depression, and anxiety.1,2 It is estimated that the prevalence of UI is 13% in women aged 18-22 years, 36% in women aged 40-49 years, and 35% in women aged 70-74 years.3 In addition to the high prevalence rate of UI especially in women, it is considered as an important social health problem that affects daily activities and quality of life.4-6 This problem affects the physical, mental, and sexual aspects of a person and causes deprivation of social status and decreases quality of life and self-confidence.7,8
In the past, surgery was the main treatment for patients suffering UI and stress urinary incontinence (SUI); recently, however conservative management has been considered as the first line of treatment for uncomplicated UI by the International Continence Society.9 Several treatment options for the management of SUI include physical therapies, pharmacological intervention and behavioral modification.9 Physical therapies involving pelvic floor muscle training (PFMT) with or without other treatments such as vaginal cones, biofeedback, and electrical stimulation are the standard techniques for treatment and prevention of SUI.10 Oh and colleagues have evaluated the effect of behavioral intervention program (BIP) including urinary incontinence education, pelvic floor muscle exercise, and bladder training, on SUI and mixed urinary incontinence and concluded that BIP for 9 weeks could significantly improve the pelvic floor muscle strength and psycho-social well-being related to urinary incontinence.11 In another study, BQ and colleagues proposed that special devices such as vaginal cones, biofeedback or electrical stimulation could make PFMT more accurate and effective. However, the researchers concluded that PFMT is superior to vaginal cones, biofeedback and electrical stimulation, and all these methods were more effective than no treatment.12 Kashanian et al. in another study compared PFMT with and without Kegelmaster device and found no difference between the two methods in improving SUI and mixed incontinence, but stated that both methods were effective.9 In a review article, Moore indicated that biofeedback therapy (electrical stimulation and weighted vaginal cones) has a variable effect on the treatment of stress urinary incontinence.13
Considering the different results in previous studies and because the Quality of Life is increasingly being used as a primary outcome measure in studies to evaluate the effectiveness of treatment,14 the present study was done to compare the effectiveness of behavioral intervention program and vaginal cones on SUI and its related quality of life.
Methods
This single-blind, randomized clinical trial was conducted at Emam Reza and Ghaem Hospitals, Mashhad University of Medical Sciences, from April 2008 to December 2009. The study protocol (Project No.85235) was approved by the Institutional Review Board and Ethics Committee at Mashhad University of Medical Sciences, and was performed in accordance with the Declaration of Helsinki. A written informed consent was obtained from all participants and they were informed about the study. Sixty women aged 25-65 years with proven stress urinary incontinence enrolled in this study. All subjects had symptoms of SUI with at least three episodes per week. Exclusion criteria included patients with chronic degenerative diseases that would affect muscular and nerve tissues, vulvovaginitis, atrophic vaginitis, pregnancy, active or recurrent urinary tract infections, advanced genital prolapses and patients with cardiac pacemakers.
The subjects were randomly assigned into two groups using 4 parts block randomization with sealed envelopes. Since the exercises were different in the two groups, blinding was not possible, but those who assessed the outcomes were blinded to group assignment. Each participants was admitted after two primary assessment sessions. Q-tip test, bladder sonography and complete urine examination were performed during the first session. In addition, the ability of pelvic floor contraction was determined and the frequency and volume charts were given to the subjects to complete for the following 3 days using a measured container (150 cc).
For the Behavioral Intervention group, the program was comprised of urinary incontinence education, PFM exercise and bladder training. The contents of the education program included the causes, symptoms, diagnoses, and treatment of urinary incontinence, the locations and functions of PFM, and methods of PFM exercise and bladder training. The patients in this group learned about the pelvic floor muscles during the determination of the active and passive cones and examination of the strength of the pelvic floor muscles, and then they were asked to contract the pelvic floor muscles and hold for 10 seconds and then relax for 10 seconds, i.e., ‘quick and hold’ contractions. The PFM exercise used in the present study was employed by the previous study by Oh and colleagues.12
According to the literature, the most prevalent contraction holding time was in the range of 4 to 30 seconds. This contraction-relaxation was repeated 10 times a day during the first week, and increased to 20, 30, and 40 times a day during the second, third, and fourth weeks, respectively. The whole exercise procedure was recorded on audiocassette tape or compact disc, and it was emphasized to the patients to perform exercises in the four positions (lying back, lying behind the stomach with feet together, standing, and kneeling) two times daily by using pamphlet and audiocassette tape. After 2 weeks of treatment, when pelvic muscles had become stronger and the exercise regime was formed, the subjects were encouraged to perform "stress strategy" and "urgency strategy", that is, they were instructed to contract pelvic muscles during activities that commonly resulted in incontinence. For stress strategy, they were instructed to contract pelvic muscles 3-4 times for 6-12 seconds duration when making an effort like sneezing, laughing, or running and lifting heavy objects. The contractions were to be performed at the time of the activities or just before in order to make the relation between the effort and the stronger pelvic muscle contraction. For urgency strategy, instead of running to void as soon as they felt the urge to urinate (which in turn, causes bladder pressure and increases the chances of leakages), participants were told to sit down (if possible), relax and contract pelvic muscles repeatedly to reduce the urgency and detrusor muscle contraction. They tried not to void until the sense of urge disappeared, after which they should urinate normally.15 The bladder training method used in the present study was explained by Oh and colleagues with the aim of extending the voluntary voiding intervals gradually every week until the voiding interval reached 3-4 hours.12
Vaginal cones are stainless steel devices with a plastic coating and a nylon thread at their apex to facilitate their removal. A set of 6 cones with similar shape and volume was used, numbered from 1 to 6 and weighing 20, 30, 40, 50, 60, and 70 grams, respectively (Weighted Mahbel Cones, Iran). Each patient started with the heaviest cone that they could hold in their vagina with the apex pointing toward the pelvic floor in a standing position. The sensation of losing the cone induced involuntary contractions of the pelvic floor musculature; the patient was then instructed to walk and not to contract her pelvic floor musculature for one minute and to report any sensation of losing the device; the number of that particular cone was considered as the passive cone.15 The subject was instructed to walk for 15 minutes twice a day with the passive cone in her vagina without voluntarily contracting her pelvic floor muscles. When the patient no longer felt the cone was falling from her vagina, the next heaviest cone was used. This procedure was continued for three months. The individual cone that the patient was able to keep in her vagina with voluntary contraction of the pelvic floor muscles for a special time was identified as the active cone. If the patient ended the passive phase with cone number 6, she would start the active phase with the same number device. After identifying the ‘‘active cone’’, the patient was trained to perform 30 voluntary contractions of 5 seconds each, alternating with 5 seconds of relaxation, twice a day, in a standing position.15 The patients were evaluated every 2 weeks by the investigator to determine whether they were using the vaginal cones correctly. The women from both groups were monitored by telephone twice a week and attended the hospital every 2 weeks to ensure the accuracy and consistency of the method.
The information related to demographic characteristics (age, age of marriage, life style, parity, number of previous cesareans, menopause status, and menopause duration), and the result of frequency and volume charts were evaluated before intervention. The subjective changes in severity of stress urinary incontinence (SUI) were measured by a questionnaire to determine the severity of SUI, leakage index, frequency, and volume chart. The leakage index was also assessed using Persian version of leakage index scale which was evaluated in a study by BQ et al.12 This is a 5-point scale (5 always, 4 often, 3 sometimes, 2 seldom, 1 never) designed to assess how often subjects experienced wet episodes in 8 special situations (sneezing, coughing, laughing, walking, walking downhill, running, jumping, and lifting) verified as the most predictable situations to induce urine leakage. The mean was calculated as an index of leakage frequency before and after treatment. The content validity and the reliability has also been examined on a number of occasions and during the present study (Cronbach=0.86-0.89). Urine loss was evaluated using the 1-hour pad test with a standardized bladder volume when 250 mL was introduced by catheter into the bladder.16,17 Pad weights were measured in grams with a valid digital scale. An increase of up to 2 g in the pad test was considered normal. Increases of 2 to 10 g were considered to be mild to moderate, 10 to 50 g severe, and above 50 g very severe.3 Pelvic floor muscle function was evaluated according to the brink scale.18,19 The Brink scale is a commonly used digital assessment of pelvic floor muscle strength. The Brink assessment was performed by placing 2 fingers vaginally during a single Kegel contraction. Brink scores consisted of 3 separate 4-point rating scales for pressure, vertical finger displacement, and duration.18
For better evaluation of their effects, 2 questionnaires of Incontinence Quality of Life (IQOL) and King’s Health Questionnaire (KHQ) were used for the evaluation of the quality of life and its improvement. After treatment of UI, different questionnaires have been suggested, and one of the most appropriate is the incontinence quality of life (IQOL) which has been approved for the Iranian population according to its validity and reliability.20 The King’s Health Questionnaire evaluates the impact of lower urinary tract symptoms on women’s quality of life and comprises 21 questions divided into eight domains such as: general health perception, incontinence impact, role limitations, physical and social limitations, personal relationships, emotions, and sleep/energy. Each KHQ domain obtains a score and, therefore, there is no general score. The scores range from 0 to 100 and the higher the score, the poorer the quality of life.21 IQOL, KHQ, brink score, severity of SUI, leakage index, and weight of active and passive cones were determined before entering the study and were again determined 8 and 12 weeks after finishing the intervention in the two groups. The specialist performing the initial and final evaluations and statistical analyses were not informed about the type of intervention to which the patients were allocated.
The data was analyzed using the SPSS software (version 13). Chi-square, Fisher exact, Mann-Whitney, and Wilcoxone tests were used for qualitative and quantitative variables with abnormal distribution variables. Student t-test and Paired t-test were applied for quantitative variables with normal distribution. A p-value of ≤0.05 was considered statistically significant.
Results
A total of 60 women enrolled into this study considering the inclusion criteria. Among them, 51 women completed the study with 25 cases in vaginal cones group and 26 in behavioral intervention program group. The other 9 patients were excluded from the study for different reasons such as irregular bleeding (2 patients), the incidence of Candida infection (3 patients) in vaginal cones group and 4 patients in the behavioral program group for failure to participate in weekly follow-up or perform regular PFM exercise.
The data in Table 1 demonstrates that there was no statistically significant difference in terms of age, BMI, parity, mode of delivery, menopause status, educational status, duration of UI, and other basic characteristics between the two groups. Also as shown in Table 2, the two groups did not indicate any statistical differences according to basic severity of SUI, leakage index, urine leakage in the 1-hour pad test, daytime urinary frequency, night time urinary frequency, and the urinary incontinence during the seven days before intervention. Decreased leakage rate on pad test was observed in both groups after 8 and 12 weeks of intervention (p<0.001, p<0.001). The changes in leakage rate on pad test in the behavioral intervention group were higher than in the vaginal cones group (p=0.008). Moreover, leakage index decreased significantly in both groups after 8 and 12 weeks of intervention (p=0.001, p=0.001). The changes in leakage index in the behavioral intervention group were higher as compared to the vaginal cone group after 12 weeks intervention (p=0.001). Although the severity of SUI decreased significantly in both groups after 8 and 12 weeks of intervention (p<0.001, p<0.001), there was no significant difference between the two groups when they were compared in terms of the changes in severity of SUI (p=0.2), as shown in Table 2.
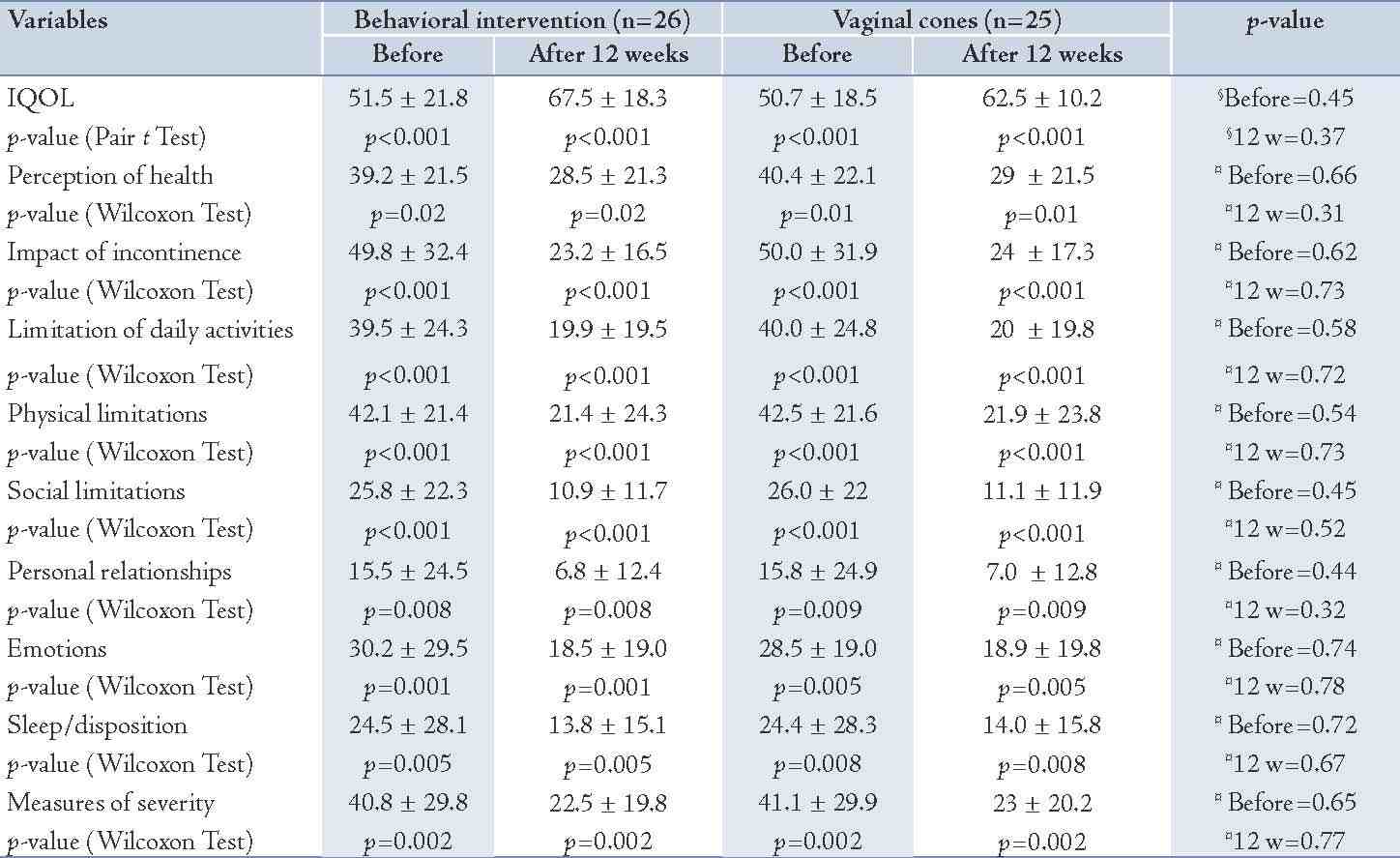
The pelvic muscle strength before intervention included the brink score. Weight of passive and active cones showed no significant differences between the two groups. These variables showed a significant improvement after 8 and 12 weeks of intervention in both groups (p<0.001), but there were no significant differences between the two groups in terms of improvement in these variables (Table 3). The quality of life scores in terms of IQOL and KHQ scores showed no significant differences between the two groups before intervention, although these scores showed significant improvement after 12 weeks of intervention. No significant difference was found between the groups according to the improvement in different scores. (Table 4)
Table 1: The demographic and SUI characteristics of the study population.
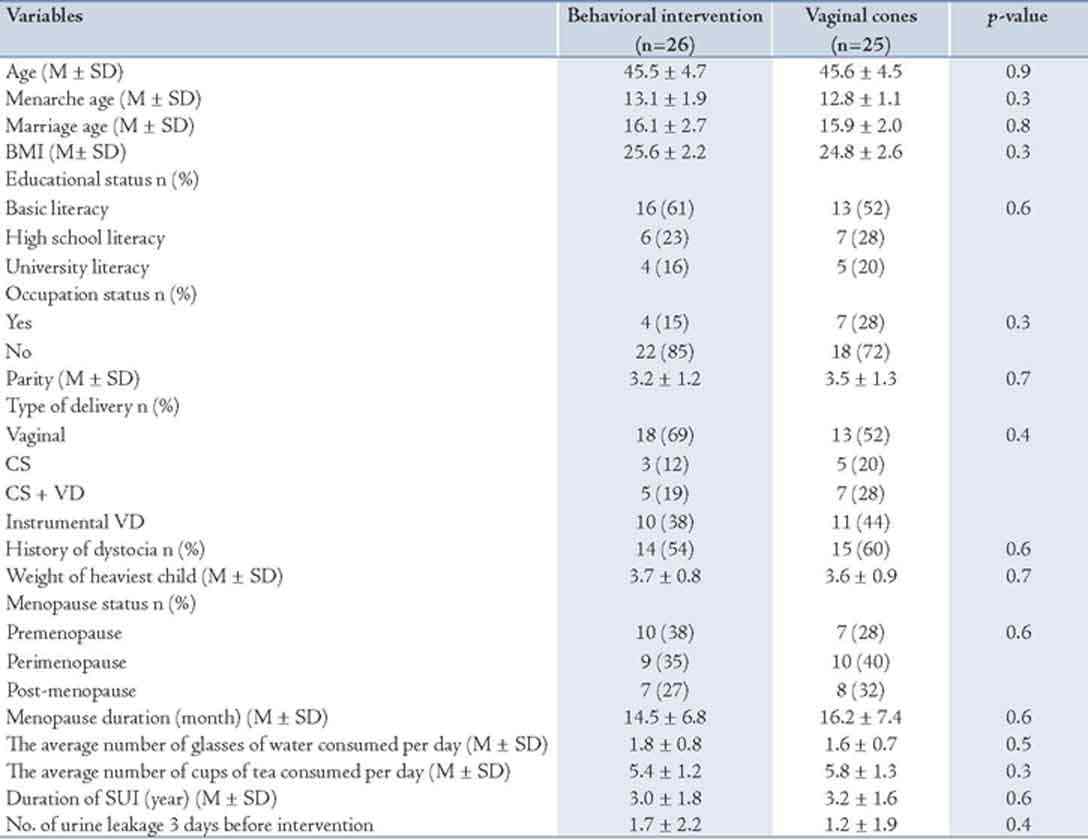
Table 2: The characteristics of SUI and pelvic floor strength of the study population.
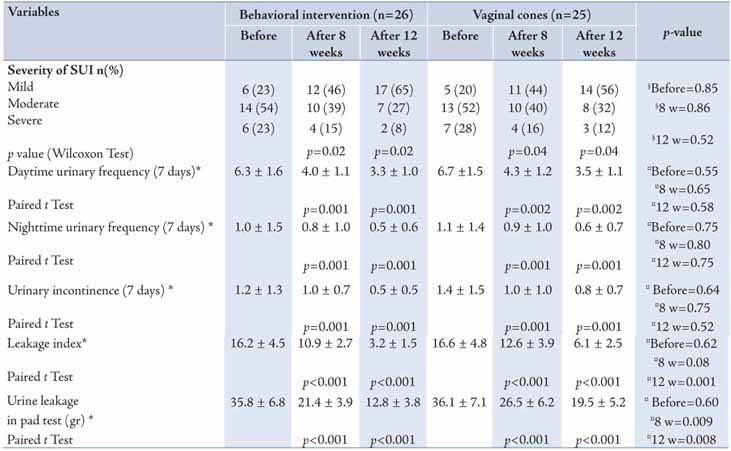
Table 3: The comparison of pelvic floor strength between the two groups.
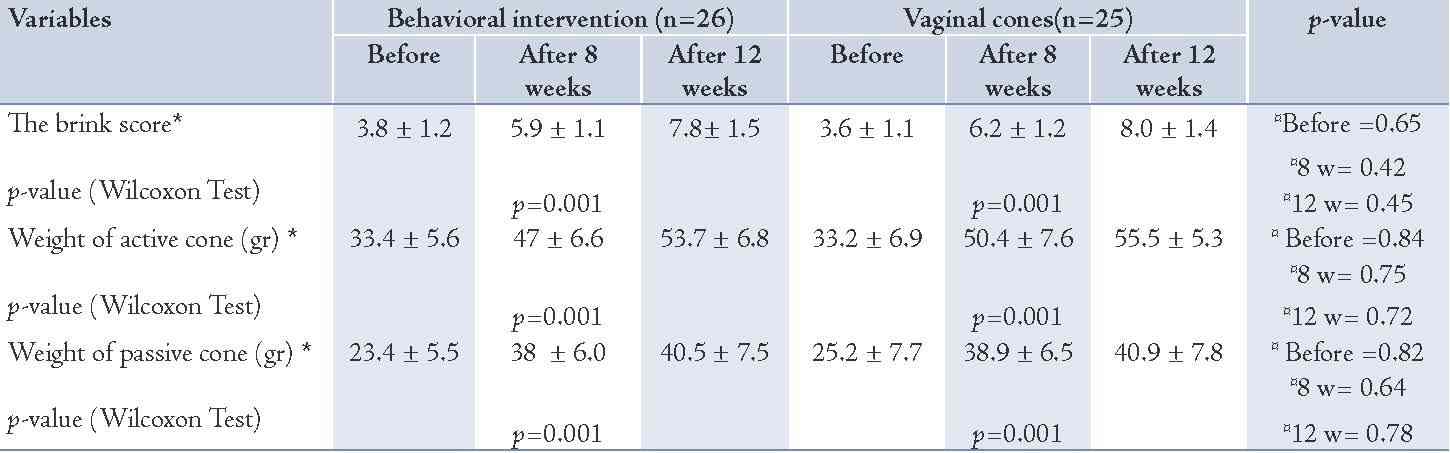
Table 4: Comparison of IQOL and KHQ scores according to the domains of KHQ before and 12 weeks after treatment between the two groups.
Discussion
Although many studies have reported the effect of PFMT on any kind of urinary incontinence, especially in young women and SUI type,22,23 in terms of comparing the effect of PFM alone with assisted PFMT like vaginal weight cones, results are still controversial.24-27
This study was performed to compare the effectiveness of PFMT in the form of a behavioral intervention program and assisted form (vaginal cones) on stress urinary incontinence. As shown in the present study, vaginal cones and behavioral intervention program both have considerable effects on the treatment of mild-to-severe stress urinary incontinence, which is comparable with some previous studies.13,15,16,26 However, the behavioral intervention program is preferred over vaginal cones when these two methods of treatment are compared in terms of leakage rate, leakage index, cost, and side effects. Also, both methods were effective with the same efficacy in improvement of quality of life related to urinary incontinence, in agreement with previous studies.9,11,28,29 The efficacy of the behavioral intervention program was evaluated in a few studies and the results of the current study are in agreement with the findings of previous studies.11,30,31 Some previous studies evaluated the effectiveness of pelvic floor exercises alone, pelvic floor exercises with biofeedback, and vaginal cones or balloon and reported no significant difference between the two groups in terms of the changes in the symptoms of stress urinary incontinence.9,17,24-26 The results of these studies are in contrast to the present findings. Goode et al. in one study reported that treatment with pelvic floor electrical stimulation did not increase effectiveness of a comprehensive behavioral program for women with stress incontinence.31
In the current study, the production of each set of vaginal cones cost $40 vs. $5 in the behavioral intervention program group for preparing instructional pamphlet and audiocassette tape or compact disc. It appears that the behavioral intervention program is a more cost-effective method in comparison to vaginal cones because it had better or similar efficacy in some variables as the vaginal cones but at a lower cost. Based on the present results, it seems that the detection of pelvic floor muscles, performing the daily activities as well as the exact follow-up, and encouraging the patients to carry out specific strategies to change their lifestyle in a behavioral program are more effective than performing exercises only with a device that exactly identify the pelvic floor muscles. Also, five cases in the vaginal cones group reported some side effects such as Candida vaginitis and difficulty in using the devices. In general, the patients’ full satisfaction was lower compared with the behavioral intervention program group (70% vs. 50%).
The limitation of this study is that the analysis in this paper was not done on an "intention to treat" analysis for prevention of bias. In the published CONSORT 2010, its explanatory document reported that strict intention-to-treat analysis is often hard to perform for two main reasons: missing outcomes for some participants and non-adherence to the trial protocol.32 In this study, four patients were excluded due to non-adherence to the protocol and five patients were omitted due to intervention withdrawal. The term "modified intention-to-treat" is commonly used to explain an analysis that excludes participants who did not adequately adhere to the protocol, specifically those who did not receive a defined minimum amount of the intervention, thus in present study, this method was used for analysis.33
Conclusion
The present study concludes that vaginal cones and behavioral intervention program both have significant effects on the treatment of mild-to-severe stress urinary incontinence. However, based on the results, the behavioral intervention program is preferred when these two methods of treatment are compared in terms of effectiveness, cost and side effects.
Acknowledgements
The authors greatly acknowledge Mansoreh Mansori (Master degree in Midwifery) for his contribution in data collection, as well as the Deputy of Research and Technology at Mashhad Medical Science University who supported this work financially. We also thank all the participants in the study. No potential conflict of interest to declare.
References
1. Doran CM, Chiarelli P, Cockburn J. Economic costs of urinary incontinence in community-dwelling Australian women. Med J Aust 2001 May;174(9):456-458.
2. Lapitan MC, Cody DJ, Grant AM. Open retropubic colposuspension for urinary incontinence in women. Cochrane Database Syst Rev 2005;(3):CD002912.
3. Ward KL, Hilton P; UK and Ireland TVT Trial Group. A prospective multicenter randomized trial of tension-free vaginal tape and colposuspension for primary urodynamic stress incontinence: two-year follow-up. Am J Obstet Gynecol 2004 Feb;190(2):324-331.
4. Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al; Standardisation Sub-Committee of the International Continence Society. The standardisation of terminology in lower urinary tract function: report from the standardisation sub-committee of the International Continence Society. Urology 2003 Jan;61(1):37-49.
5. Hunskaar S, Burgio K, Diokno A, Herzog AR, Hjälmås K, Lapitan MC. Epidemiology and natural history of urinary incontinence in women. Urology 2003 Oct;62(4)(Suppl 1):16-23.
6. Chiarelli P, Brown W, McElduff P. Leaking urine: prevalence and associated factors in Australian women. Neurourol Urodyn 1999;18(6):567-577.
7. Cardozo L. Duloxetine in the context of current needs and issues in treatment of women with stress urinary incontinence. BJOG 2006 May;113(Suppl 1):1-4.
8. Subak LL, Brown JS, Kraus SR, Brubaker L, Lin F, Richter HE, et al; Diagnostic Aspects of Incontinence Study Group. The "costs" of urinary incontinence for women. Obstet Gynecol 2006 Apr;107(4):908-916.
9. Kashanian M, Ali SS, Nazemi M, Bahasadri S. Evaluation of the effect of pelvic floor muscle training (PFMT or Kegel exercise) and assisted pelvic floor muscle training (APFMT) by a resistance device (Kegelmaster device) on the urinary incontinence in women: a randomized trial. Eur J Obstet Gynecol Reprod Biol 2011 Nov;159(1):218-223.
10. Dmchowski RR, Miklos JR, Norton PA, Zinner NR, Yalcin I, Bump RC. Duloxetine versus placebo for the treatment of North American women with stress urinary. J Urol 2004;170:1259-1263 .
11. Oh HS, Kim MK, Seo WS. Effectiveness of a behavioral intervention program for urinary incontinence in a community setting. Taehan Kanho Hakhoe Chi 2005 Dec;35(8):1476-1484.
12. Bø K, Talseth T, Holme I. Single blind, randomised controlled trial of pelvic floor exercises, electrical stimulation, vaginal cones, and no treatment in management of genuine stress incontinence in women. BMJ 1999 Feb;318(7182):487-493 BMJ 1999;318:487-493.
13. Moore KH. Conservative management for urinary incontinence. Bailer’s. Clin Obstet Gynecol 2000;14(2):251-289.
14. Dehkordi A, Heydarnejad MS, Fatehi D. Quality of Life in Cancer Patients undergoing Chemotherapy. Oman Med J 2009 Jul;24(3):204-207.
15. Santacreu M, Fernández-Ballesteros R. Evaluation of a behavioral treatment for female urinary incontinence. Clin Interv Aging 2011;6:133-139.
16. Haddad JM, Ribeiro RM, Bernardo WM, Abrão MS, Baracat EC. Vaginal cone use in passive and active phases in patients with stress urinary incontinence. Clinics (Sao Paulo) 2011;66(5):785-791.
17. Cammu H, Van Nylen M. Pelvic floor exercises versus vaginal weight cones in genuine stress incontinence. Eur J Obstet Gynecol Reprod Biol 1998 Mar;77(1):89-93.
18. Brink CA, Wells TJ, Sampselle CM, Taillie ER, Mayer R. A digital test for pelvic muscle strength in women with urinary incontinence. Nurs Res 1994 Nov-Dec;43(6):352-356.
19. Hundley AF, Wu JM, Visco AG. A comparison of perineometer to brink score for assessment of pelvic floor muscle strength. Am J Obstet Gynecol 2005 May;192(5):1583-1591.
20. Nojomi M, Baharvand P, Moradi Lakeh M, Patrick DL. Incontinence quality of life questionnaire (I-QOL): translation and validation study of the Iranian version. Int Urogynecol J Pelvic Floor Dysfunct 2009 May;20(5):575-579.
21. Kelleher CJ, Cardozo LD, Khullar V, Salvatore S. A new questionnaire to assess the quality of life of urinary incontinent women. Br J Obstet Gynaecol 1997 Dec;104(12):1374-1379.
22. Dumoulin C, Hay-Smith J. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database Syst Rev 2010;1(1):CD005654.
23. Hay-Smith EJ, Dumoulin C. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database Syst Rev 2006;1(1):CD005654.
24. Gameiro MO, Moreira EH, Gameiro FO, Moreno JC, Padovani CR, Amaro JL. Vaginal weight cone versus assisted pelvic floor muscle training in the treatment of female urinary incontinence. A prospective, single-blind, randomized trial. Int Urogynecol J 2010 Apr;21(4):395-399.
25. Ferguson KL, McKey PL, Bishop KR, Kloen P, Verheul JB, Dougherty MC. Stress urinary incontinence: effect of pelvic muscle exercise. Obstet Gynecol 1990 Apr;75(4):671-675.
26. Castro RA, Arruda RM, Zanetti MR, Santos PD, Sartori MG, Girão MJ. Single-blind, randomized, controlled trial of pelvic floor muscle training, electrical stimulation, vaginal cones, and no active treatment in the management of stress urinary incontinence. Clinics (Sao Paulo) 2008 Aug;63(4):465-472.
27. Mørkved S, Bø K, Fjørtoft T. Effect of adding biofeedback to pelvic floor muscle training to treat urodynamic stress incontinence. Obstet Gynecol 2002 Oct;100(4):730-739.
28. Rivalta M, Sighinolfi MC, Micali S, De Stefani S, Bianchi G. Sexual function and quality of life in women with urinary incontinence treated by a complete pelvic floor rehabilitation program (biofeedback, functional electrical stimulation, pelvic floor muscles exercises, and vaginal cones). J Sex Med 2010 Mar;7(3):1200-1208.
29. Fitz FF, Costa TF, Yamamoto DM, Resende AP, Stüpp L, Sartori MG, et al. Impact of pelvic floor muscle training on the quality of life in women with urinary incontinence. Rev Assoc Med Bras 2012 Mar-Apr;58(2):155-159.
30. Subak LL, Quesenberry CP, Posner SF, Cattolica E, Soghikian K. The effect of behavioral therapy on urinary incontinence: a randomized controlled trial. Obstet Gynecol 2002 l Jul;100(1):72-78.
31. Goode PS, Burgio KL, Locher JL, Roth DL, Umlauf MG, Richter HE, et al. Effect of behavioral training with or without pelvic floor electrical stimulation on stress incontinence in women: a randomized controlled trial. JAMA 2003 Jul;290(3):345-352.
32. Schulz KF, Altman DG, Moher D; CONSORT Group. CONSORT 2010 statement: updated guidelines for reporting parallel group randomized trials. Ann Intern Med 2010 Jun;152(11):726-732.
33. Abraha I, Montedori A, Romagnoli C. Modified intention to treat: frequency, definition and implication for clinical trials [abstract]. Sao Paulo, Brazil: XV Cochrane Colloquium. 2007: 86-87.
|