| |
Abstract
Hepatocellular carcinoma is the most frequent type of liver malignancy. Most cases of hepatocellular carcinoma are secondary to either viral hepatitis (hepatitis B, C) or alcoholic cirrhosis. Liver cirrhosis due to any other causes is considered as a risk factor for development of hepatocellular carcinoma; however, hepatocellular carcinoma in a young patient with no cirrhosis or fibrosis is a relatively rare condition. The present case report describes a young 24-years-old male patient who presented with a two-month history of fever, right upper quadrant abdominal pain, and weight loss with no evidence of pre-existing liver disease, initially treated as liver abscess; however, a computed tomography (CT) showed numerous hepatic hypodensities with ring enhancement. Serum alpha-fetoprotein level was high (>1000 ng/L) and histopathological study confirmed the presence of primary hepatocellular carcinoma. The present case findings suggest that multifocal hepatocellular carcinoma can occur in a young patient with no apparent risk factor, and that the clinical presentation of hepatocellular carcinoma can be similar to liver abscess.
Keywords: Hepatocellular carcinoma; Liver abscess; Chronic liver disease.
Introduction
Hepatocellular carcinoma (HCC) is the most frequent type of malignant lesion of the liver. Liver cancer can rarely occur below the age of 40 years and reaches a peak at approximately 70 years. Rates of HCC among men are two to four times as high as the rates among women.1 Although not frequently, HCC can occur in a non-cirrhotic liver. In comparison with cirrhotic HCC, non-cirrhotic HCC has some characteristics, such as: (a) a lower male preponderance and a bimodal age distribution; (b) a lower prevalence of the three major risk factors (hepatitis B and C virus infections and alcohol abuse), with an increased prevalence of other etiologies, such as exposure to genotoxic substances and sex hormones, inherited diseases, genetic mutations; (c) a more advanced tumor at the time of diagnosis, as it is usually detected due to the occurrence of cancer-related symptoms, outside any scheduled surveillance program.2
Case Report
A 24-year-old patient was admitted to our hospital with a 2-month history of right hypochondriac pain and fever. He also reported decreased appetite, significant weight loss, and occasional vomiting but there were no other symptoms. He gave no history of chronic medical illnesses; there was no drug or family history of note. He denied cigarette smoking or alcohol consumption. Before presenting here, the patient was already previously seen in another hospital in which a diagnosis of liver abscess was made.
On examination, he appeared sick, jaundiced and febrile, with a body temperature of 38.5°C. Abdominal examination revealed a palpable liver (10 cm below the right costal margin, irregular, firm and tender), no splenomegaly or ascites. He had no peripheral stigmata of chronic liver disease, neither signs of hepatic failure. Examination of other systems was unremarkable. Accordingly during admission, intravenous antibiotics (in the form of ceftriaxone and metronidazole) were given without improvement. Abdominal ultra-sonogram was done and showed multiple hypodense hepatic lesions; otherwise, there were no signs of portal hypertension or ascites. A computed tomography (CT) revealed multiple hypodense hepatic lesions with ring enhancement (Fig. 1). Serum alpha-fetoprotein level was >1000 ng/L (normal <3 ng/L). Histopathological study of liver specimen reported poorly differentiated malignant cells consistent with hepatocellular carcinoma (Fig. 2). CBC revealed a Hb of 14.6 gm/dL, WBC of 11300/cmm, and platelets of 291,000/cmm. LFTs showed total bilirubin of 35 mmol/L (reference range 0-17), ALT 54 IU/L (30-65), AST 74 U/L (15-37), alkaline phosphatase 344 U/L (50-136), GGT 646 U/L (1-94), total protein 64 g/L (64-82), albumin 33 g/L (34-50). PT and PTT were normal. Serology for viral hepatitis including HBsAg, HBcAb, and HCV-Ab was negative. Also, PCR for HBV-DNA was negative. Iron panel was normal. RFTs and electrolytes were normal except for hypercalcemia (serum Ca++ of 3.32 mmol/L), but PTH and phosphate were normal.
Septic workup including urine and blood culture showed no evidence of infection. Metastatic workup including PSA and CEA levels, chest-x-ray, chest CT scan, bone scan, upper and lower GI endoscopies were all normal. He received only symptomatic treatment and a decision was made to refer him to a higher hepatology centre for further management, but the patient preferred to go to his native country.

Figure 1: CT revealed multiple hypodense hepatic lesions with ring enhancement.
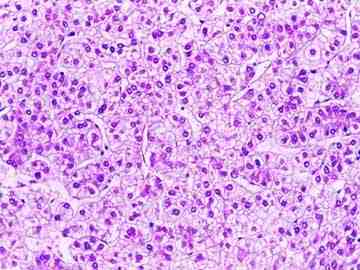
Figure 2: Histopathological study of liver specimen with poorly differentiated malignant cells consistent with hepatocellular carcinoma
Discussion
Hepatocellular carcinoma (HCC) is the common type of primary liver cancer. HCC has an annual incidence of 600,000 newly diagnosed patients. Thus, HCC constitutes the sixth most frequent form of cancer worldwide and it holds third place in terms of malignancy-related mortality. Eighty percent (80%) of liver cancers are found in cirrhotic livers, which themselves carry a high risk for HCC.3 HCC in a young patient with no cirrhosis or fibrosis is a relatively rare diagnosis.4 This is compatible with the presented case as the patient showed no evidence of pre-existing liver disease. Clinical presentation of the patient was similar to liver abscess in view of fever, right hypochondrial pain and leukocytosis. Few similar cases of HCC mimicking liver abscess were reported by Yeom et al and Hayashi et al.5,6 HCC in adults is largely a disease common among those 50-70 years old; however, there is a type of HCC with characteristic histological features that usually occurs in young adults known as fibrolamellar hepatocellular carcinoma (FHCC). FHCC is rich in fibrous tissue with males and females being at equal risk. It does not produce alpha-fetoprotein and it has a good prognosis.7
The age of the patient and lack of coexisting liver disease favor the diagnosis of FHCC, but the radiological and histological findings in addition to high alpha-fetoprotein level are against such diagnosis. Pathologically, HCC can be either single or occur as multiple nodules throughout the liver. Histologically, it consists of cells resembling hepatocytes. It can metastasize via the hepatic or portal veins to the lymph node, bones and lungs.8 For this patient, the histopathological studies revealed malignant cells consistent with HCC. The presence of hypercalcemia in the patient can be part of paraneoblastic manifestations of HCC. He had normal serum PTH and phosphorus levels (ruling out the possibility of primary hyperparathyroidism), and his metastatic workup showed no evidence of bone disease. Some cases of severe hypercalcemia associated with HCC were reported, in which the cause of hypercalcemia was ectopic PTH-related peptide secretion. This type of hypercalcemia usually responds to treatment of the underlying tumor.9,10
HCC on CT scan may appear as focal lesion which can invade the portal or hepatic veins. It can also be multifocal or may be found diffusely in the liver. It usually has a heterogeneous appearance. On CT and MRI, it typically enhances more than the adjacent liver after the intravenous contrast is administered especially if the liver is imaged within 20 seconds after contrast is given (during the hepatic arterial phase of contrast enhancement of the liver since HCC is a hypervascular cancer and is fed by hepatic artery.11
Patients with HCC diagnosed at an early stage are optimal candidates for resection, liver transplantation or percutaneous ablation. Surgical resection is recommended for patients with single tumors, absence of clinically relevant portal hypertension and normal bilirubin. Transplantation is indicated in patients with 3 nodules of <3 cm or with single tumors <5 cm with liver function impairment precluding resection. Transarterial chemoembolization (TACE) is recommended in asymptomatic patients with multinodular tumors that have not invaded hepatic vessels nor been disseminated outside the liver. Sorafenib is indicated as the first line of treatment in patients who cannot benefit from the above therapeutic options and still have a preserved liver function.12,13 Finally, the rare clinical presentation and the age of the patient at the time of presentation are the interesting features of the case.
Conclusion
Although HCC is common worldwide especially in areas in which there is a high prevalence of viral hepatitis B and C, multifocal HCC in young adults without clear risk factors is an extremely rare case.
Acknowledgements
The authors report no conflict of interest and no funding was received for this work.
References
1. El-serag H. Hepatocellular carcinoma: review article. N Eng. J Med 2011;365:1118-1127.
2. Trevisani F, Frigerio M, Santi V, Grignaschi A, Bernardi M. Hepatocellular carcinoma in non-cirrhotic liver: a reappraisal. Dig Liver Dis 2010 May;42(5):341-347.
3. Mauss S, Berg T, Rockstroh J, Sarrazin C, Wedemeyer H. Hepatocellular carcinoma, Hepatology-a clinical text book,2ed edition. Germany: Flying publisher 2010,P 303-304
4. Thomas DB, Hall AB, Michel M. Non-cirrhotic hepatocellular carcinoma in a young active duty male. Mil Med 2011 Apr;176(4):475-476.
5. Yeom JO, Yoon SB, Kim JG, Oh JH, Jeon EJ, Jeong et al. a case of hepatocellular carcinoma combined with Liver abscess. korean. J Gastroenterol 2009;53:378-382.
6. Hayashi T, Honda H, Kaneko K, Fukuya T, Tateshi Y, Ro T, et al. Hepatocellular carcinoma with pyrexia: report of a case. Radiat Med 1995 May-Jun;13(3):133-136.
7. Terzis I, Haritanti A, Economou I. Fibrolamellar hepatocellular Carcinoma: a case report with distinct radiological features. J gastrointestinal. Cancer 2010;41:2-5.
8. Kumar P, Clark M. Hepatocellular carcinoma. Clinical Medicine, 5th ed. Toronto: W. B Saunder 2002; p: 384.
9. Abe Y, Makiyama H, Fujita Y, Tachibana Y, Kamada G, Uebayashi M. Severe hypercalcemia associated with hepatocellular carcinoma secreting intact parathyroid hormone: a case report. Intern Med 2011;50(4):329-333.
10. Ghobrial MW, George J, Mannam S, Henien SR. Severe hypercalcemia as an initial presenting manifestation of hepatocellular carcinoma. Can J Gastroenterol 2002 Sep;16(9):607-609.
11. Douglas S, Kevin R, Stuart A. Liver disease. Radiology secrets.1st edition. USA: Amazon.com 1998, P132.
12. T, Meloni F, Di Stasi M, Rolle E, Solbiati L, Tinelli C, et al. Sustained complete response and complications rates after radiofrequency ablation of very early hepatocellular carcinoma in cirrhosis: Is resection still the treatment of choice? HEPATOLOGY 2008; 47: 82-89.
13. Llovet JM, Ricci S, Mazzaferro V, Hilgard P, Gane E, Blanc JF, et al; SHARP Investigators Study Group. Sorafenib in advanced hepatocellular carcinoma. N Engl J Med 2008 Jul;359(4):378-390.
|