|
Abstract
Objective: Malaria is today one of the major causes of human suffering, both in terms of increasing morbidity/mortality and stunting intellectual/ economic growth. In a developing country like India, it has devastating socioeconomic consequences. The present study was therefore carried out to study the epidemiology of malaria in Amritsar district.
Methods: Diagnosed cases of Malaria reported from 1st January to 31st December 2009 in the erstwhile District of Amritsar were collected from the District Epidemiologist of Amritsar and Taran Taaran and studied. A total of 314 patients were studied. Data was assessed, systematically compiled and statistically analyzed.
Results: Most (84%) of the malaria patients in our study were less than 45 years of age. Male patients (57%) outnumbered females (43%). The majority of patients with malaria (98%) were from rural areas and 68.5% of the studied patients belonged to upper lower socioeconomical class according to Kuppuswamy socioeconomic status scale. The majority (83%) of patients took treatment from Registered Medical Practitioners/quacks. Out of the total patients, only 14% used mosquito nets, 13% used repellents, and 7% had wire gauze doors in their homes
Conclusion: The people living in rural areas were found to be more vulnerable to malaria. The disease was found to be more prevalent among the lower socio economic strata and young population leading to considerable adverse effect on health and economy. Our study aims to stress the estimation of the true burden of malaria.
Keywords: Epidemiology; Amritsar; Malaria; India.
Introduction
Vector borne disease is a type of disease where the pathogenic microorganism is transmitted from an infected individual to another individual by an arthropod or other agent, sometimes with other animal serving as an intermediate host.1 Vector borne diseases are today one of the major causes of human suffering, both in terms of increasing morbidity/mortality and stunting intellectual/ economic growth. No country, whether tropic or temperate and developed or underdeveloped, is spared from their devastating impact.2
The two most important factors related to a vector transmission of disease are the geographic range (both in distance and in amount of time during the year that the vector is present) and the vector rate of infectivity by any parasite.3 Out of the Vector Borne diseases one of the important disease is Malaria, which has been a scourge for mankind for centuries. During the pre eradication era, the estimated malaria morbidity and mortality was around 75 million and 0.75 million respectively.4 During the eradication era, with the evolvement of programs such as National Malaria control program in 1953 and then the National Malaria eradication program in 1958, India achieved tremendous success till 1965.4 But after early success the program began to face difficulties. This resulted in deterioration of the situation with focal outbreaks which necessitated reversion of many areas from consolidation phase to attack phase. The resurgence of Malaria in Asia in the late 1960s and early 1970s provides a dramatic example of how quickly malaria trends can change.4 Cases of falciparum malaria were almost negligible during 1960’s; however, the number rose to 48% of the total reported malaria cases in 2002 and around 50% in last 2-3 years.5 In India and many other tropical countries, approximately 2 to 3 million new cases arise every year.6
The picture which emerges is clear that malaria which was once under control or was endemic to certain areas is now emerging as an epidemic disease. The reasons may be reluctance in control measures or other policies related to breeding places of these vectors or migration of people, etc. Socioeconomic conditions of the community have direct bearing on the problem of these diseases. Ignorance and impoverished conditions of people contribute towards creating breeding grounds and spread of these vector borne diseases and hinder disease control strategy.7-10
Health departments hold various health education campaigns against these diseases, where a separate component for health education has been established. At district level, there is mass education and information wing, which is to perform health education programs in the form of lectures and exhibitions related to health. At PHC level, a Block Extension Educator is responsible for these activities.11 However, despite various surveillance and education programs, the data available just reflects the trends and not the real burden of disease. It is observed that very few studies on the epidemiology malaria have been carried out in this part of the country, with very limited information on age and sex-specific seasonal prevalence of the disease. The present study was carried out to study the epidemiology of malaria in district Amritsar.
Methods
This study was conducted in Amritsar District (Including Taran Taaran as it was a part of erstwhile District Amritsar) from the month of January 2009 to December 2009. All the diagnosed cases of malaria reported from 1st January to 31st December 2009 in the erstwhile District of Amritsar which also included Taran Taaran, were studied. In total, 314 patients were enrolled. Information of the patients reported to be suffering from Malaria was collected by District Epidemiologists of Amritsar and Taran Taaran. These were patients who were reported by health workers to the District Health authorities after confirmation by examination of peripheral blood smears. Health workers of the area were contacted for tracing the cases. The subjects were informed about the nature and purpose of the study and informed consent was obtained. The sociodemographic characters such as name, age, sex, address, income and education level were collected. In addition, data related to disease history, type of treatment received, along with residential environment and surrounding was obtained by the author personally, by interviewing the patients through home visits.
The Various criteria used wereas follows:
Registered Medical Practitioner: A person having no professional qualification, but taken some training from some qualified doctor and opened up his clinic.
Qualified private Practitioner: A person having basic professional qualification and registered with Punjab Medical Council or Medical Council of India or any such regulatory authority.
The Kuppuswamy’s Socioeconomic Status Scale.12 was used for assessment of socioeconomic status. This scale included education, occupation and income of the family. According to this scale, five socioeconomic classes are identified:- upper, upper middle, lower middle, upper lower and lower.12
The information collected was compiled, statistically analyzed and valid conclusions were drawn. Data was statistically analyzed with Microsoft excel and epi-info. The study was approved by the Ethical Committee of the institute.
Results
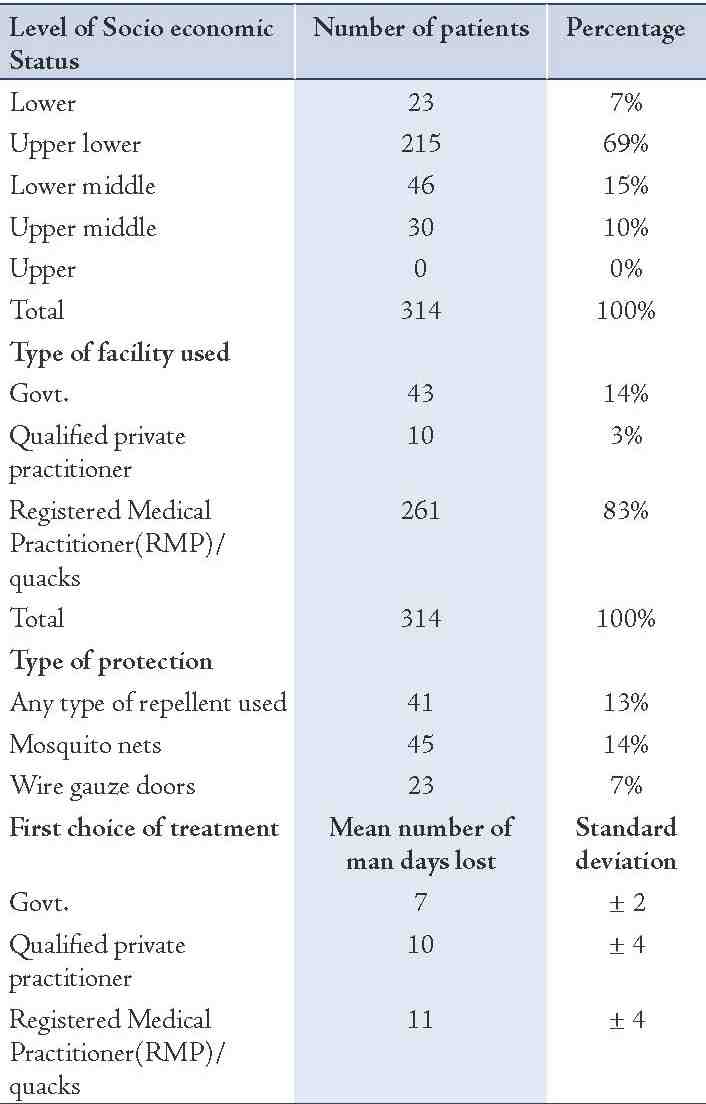
Fig. 1 shows the distribution of patients according to age group and sex. The majority of patients were from rural areas (306; 98%), while only 8 (3%) were from urban areas and belonged to the lower socioeconomic strata (Table 1). Also, the majority of patients in the current study did not use any type of protective measures against mosquito bites (Table 1). Registered medical practitioners (RMP)/quacks were the first source of treatment for majority (83%) of the patients. Table 1 also shows the distribution of Malaria patients according to the relationship between first time treatment and man days lost due to illness. The patients who received treatment from RMPs took more time for recovery than the other facilities used. The difference was found to be statistically significant (p<0.001).
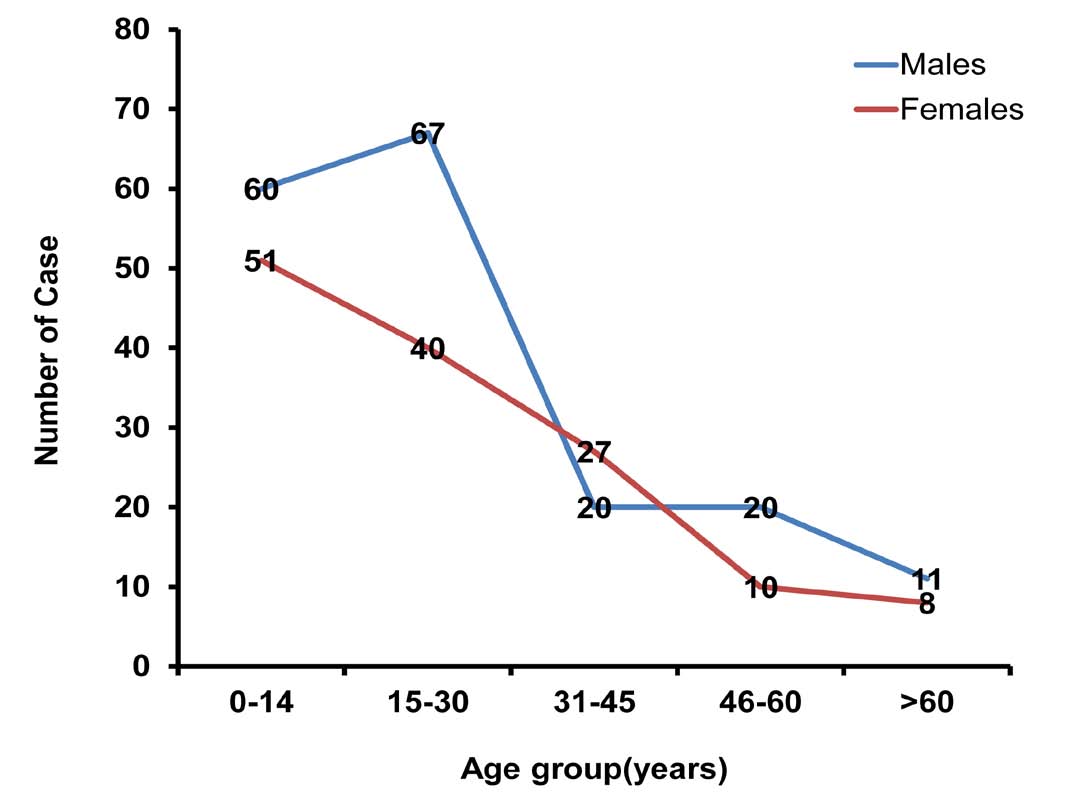
Figure 1: Distribution of Malaria patients according to age groups and sex.
Table 1: Distribution of malaria patients according to socio economi status, first contact of patients to health facility and any type of preventive measure used by these patients.
Discussion
In the present study, the majority of the patients (84%) were under the age of 45 years. In areas with high endemicity, protection among adults may be presumed to be the cumulative product of many dozens of infections, and the susceptibility of children would be due to their relative paucity of experience with infection.13 This may be the reason why this disease was more prevalent amongst the younger age group. The age group 15-45 years of the study population accounted for 49% of the total cases and deserves attention as most of the disease burden was borne by these economically productive ages. This results in significant DALY’s loss,
In our study, 178 (57%) patients were males and 136 (43%) were females. This may be attributed to more outdoor activities by males. Further, females in India are usually better clothed than males, which give them protection against mosquito bites. Other authors have also reported the disease to be more prevalent in males as compared to females. A survey on Malaria was conducted by A. Ali Karimi et al. in the south east of the Caspian sea which also showed that the proportion of disease in males was 53% and in females 47%.14
In the present study, the maximum number of patients (98%) was from rural areas. This can be attributed to more breeding of mosquitoes in rural areas because of agricultural practices being followed there,15 and breeding of mosquitoes in cattle sheds where water gets collected due to blockage of drainage by cow dung. Active surveillance of fever cases by the multipurpose health worker male is efficient in rural areas; this might also be the reason for the reporting of higher number of cases from rural areas. Moreover in rural areas, people mostly report to the public health facility for treatment, whereas in urban areas, they have access to the private practitioners and probably less number of patients report at public health facilities, thus leading to a larger number of malaria cases being reported in rural areas. This limits the exact calculation of the burden of malaria that the community has to bear, as the cases reported only represent the tip of the iceberg.16
In addition, 69% of the studied patients belonged to upper lower socioeconomical class according to Kuppuswamy socioeconomic status scale, while 46 (15%), 30 (10%) and 23 (7%) belonged to lower middle, upper middle and lower groups,12 respectively. About 75% of the patients belonged to the lower and upper lower status and this factor contributes towards their less purchasing power, so they were unable to buy mosquito nets, insect repellents and do not follow the mosquito control measures such as spraying insecticides inside the houses. The poor find it hard to deal with the persistent malaria problem, as coping with the disease is economically disastrous for the communities living on the edge. An eight-month qualitative study conducted in 1999 in four villages of Bong Tee sub district, Kanchanaburi Province located along the Thai-Myanmar border area, confirmed that poverty or difficulty in sustaining a living in the communities constantly exposed the people to malaria and caused malaria epidemics in ways such as forcing people to live without health resources and to work without protection.17
Also, 261 (83%) of patients had taken initial treatment from Registered Medical Practitioner. While, only 43 (14%) patients had taken treatment from Government Hospitals. Treatment taken from qualified private practitioner was only in 10 (3%) patients. In a study conducted by the Indian Medical Association, it was reported that out of 1000 patients going for regular treatment, 100 reach MBBS doctors, 100 reach super specialists and the rest (800) go to registered medical practitioners (quacks).18
A similar finding was also reported in the World bank study 2001, that the proportion of private expenditure on health in India is the highest in the world i.e., 84% as compared to just 16% of public expenditure.19 The majority (83%) of patients had first reported to RMPs because these RMPs are available 24 hours and live very nearby in the village, thus, making them more accessible to the community.
Conclusion
The people living in rural areas were found to be more vulnerable to malaria. The disease was found to be more prevalent among the lower socio economic strata and among the young population leading to considerable adverse effects on health and economy. Our study highlights that the present available data from different sources just represents the tip of the iceberg, thus multicentric campaigns should be encouraged to study the real epidemiology of malaria, combined with a strong political will and active community participation.
Acknowledgements
The authors reported no conflict of interest and no funding was received for this work.
References
1. Changes in the Incidence of Vector-borne Diseases Attributable to Climate Change. Ciesin Thematic Guides [Online]. [cited 2008 Oct 16]; [1 screen]. Available from: URL: htpp: //www.ciesin columbia.edu/TG/HH/veclev2. html-4k.
2. Vector born disease: Epidemiology and Control [Online].[cited 2010 Sep 26];[1 screen].Available from: URL: http://www.easternbookcorporation. com/moreinfo.php?txt_searchstring=16083
3. Longstreth J, Wiseman J. The Potential Impact of Climate Change on Patterns of Infectious Disease in the United States. Office of Policy, Planning, and Evaluation, U.S. Washington; U.S. Environmental Protection Agency; 1989. p.3, 10, 12, 16.
4. Gubler DJ. Resurgent vector-borne diseases as a global health problem. Emerg Infect Dis 1998 Jul-Sep;4(3):442-450.
5. Malaria situation in SEAR countries.India.World Health Organisation.Regional office of South-East Asia [Online]. [Cited 2010 Nov 18]; [3 screens]. Available from:URL: http://www.searo.who.int/en/Se ction10/Section21/ Section340_4021.htm.
6. Prajapati BG, Patel AK, Patel MM. Study of Hospital Based Malaria Cases in Mehsana of North Gujarat. The Internet Journal of Third World Medicine 2007;5(1):1-6.
7. Tyagi P, Roy A, Malhotra MS. Knowledge, awareness and practices towards malaria in communities of rural, semi-rural and bordering areas of east Delhi (India). J Vector Borne Dis 2005 Mar;42(1):30-35.
8. Wessen AF. Human ecology and malaria. Am J Trop Med Hyg 1972 Sep;21(5):658-662.
9. Yadav SP, Tyagi BK, Ramnath T. Knowledge, attitude and practice towards malaria in rural communities of the epidemic-prone Thar Desert, northwestern India. J Commun Dis 1999 Jun;31(2):127-136.
10. Ahorlu CK, Dunyo SK, Afari EA, Koram KA, Nkrumah FK. Malaria-related beliefs and behaviour in southern Ghana: implications for treatment, prevention and control. Trop Med Int Health 1997 May;2(5):488-499.
11. Guide HW. National Rural Health Mission. Ministry of Health and Family Welfare. Govt of India [Online]. 2010 Apr [Cited 2010 Nov 12]; [12 Screens]. Available from:URL:htpp:// www.mohfw.nic.in/nrhm.htm-56k.
12. Kumar N, Shekhar C, Kumar P, Kundu AS. Kuppuswamy’s socioeconomic status scale-updating for 2007. Indian J Pediatr 2007 Dec;74(12):1131-1132.
13. Doolan DL, Dobaño C, Baird JK. Acquired immunity to malaria. Clin Microbiol Rev 2009 Jan;22(1):13-36.
14. Zarchi AA, Mahmoodzadeh A, Vatani H. A survey on malaria and some related factors in South East of Caspian Sea. Pak J Med Sci 2006 Dec;22(4):489-492.
15. Government of Punjab. Dalits-On the margins of development. in; Human Development Report 2004, Govt of Punjab, India; pg143-53.
16. Oladeinde BH, Omoregie R, Odia I, Oladeinde OB. Prevalence of Malaria and Anemia among Pregnant Women Attending a Traditional Birth Home in Benin City, Nigeria. Oman Med J 2012 May;27(3):232-236.
17. Panvisavas S. Poverty and malaria: a study in a Thai-Myanmar border area. Southeast Asian J Trop Med Public Health 2001 Sep;32(3):608-614.
18. Too many quacks ruin a citys’ health.RTI India.org.Right to information Community Portal of India [Online]. [cited 2010 Nov 16]; [3 screens]. Available from: URL: htpp: www.imaapstate.com/ downloads/32%20anti% 20quackery.pdf.
19. Sengupta A, Joseph RK, Modi S, Syam N, eds. Economic Constraints to Access to Essential Medicines in India. New Delhi: Progressive Printers, A-21 Jhilmil Industrial Area, Shahdara. p.1-72.
|