|
Abstract
Electrical burn occurs when a current passes through the body, interfering with the function of internal organs or sometimes burning tissue. Four major mechanisms of electricity-induced injuries are presently known. In this case report, a 29-year-old farmer sustained electrical trauma to extremities from a high voltage transformer, followed by a major, deep burn wound on upper lateral aspect of his left arm, and a deep burn wound over the left medial ankle. After a few months, the patient developed left arm fracture with complete separation of two segments, and plantar wound with purulent discharge accompanied by complete destruction of the head of 4th metatarsal bone which was in favor of chronic osteomyelitis. In this case, passage of the high voltage current and direct trauma could destroy metaphyseal, medullary and periosteal blood supply. Patients with high voltage electrical-induced bone injuries who underwent reconstructive surgery seem to be susceptible to osteonecrosis and pathologic fractures; therefor, these patients should be under close follow-up and periodic radiologic evaluations may be recommended.
Keywords: Burn; Electrical injury; Spontaneous fracture.
Introduction
The discovery of electricity resulted into the promotion of industries, but led to deadly complications.1 The percentage of electrical burns varies from 3.2% in Eastern Asia to 21% in Turkey.2,3 Electrical burns occur when a current passes through the body, interfering with the function of internal organs or sometimes burning tissue.4 Low voltage injuries, caused by voltage less than 1000V, includes most injures caused by household current. High voltage, result of exposure to 1000V or more, is often resulting from occupational exposure to outside power lines. Lightening injuries involve energy with high voltage and amperage but short duration.4 Four major mechanisms of electricity induced injuries are presently known. Electrical energy can directly cause intense muscular contraction, asystole and/or apnea.5 Conversion of electrical energy into thermal energy, which can only be on the surface or may extend deep into the tissues, can cause massive tissue destruction and coagulative necrosis.
Mechanical injury with direct trauma resulting from falls or violent muscle contraction could hurt the victim.4-6 Finally, electricity can directly cause pore formation in the lipid bilayer that form the cell membrane, and allow free passage of ions and fluid; a process called electroporation.5 Severity of injury is determined by the type of circuit and current, voltage of circuit, amperage of circuit, pathway of current through the body, and the duration of contact.4-6
Case Report
On March 20, 2009, a 29-year-old farmer sustained electrical trauma to extremities from a high voltage transformer, followed by falling down from electrical post. The patient had an exit 4th degree burn wound, 25 × 15 cm, on upper lateral aspect of left arm with necrotic tissue and exposed burned-cortex humerus (entrance wound), and a deep wound over left medial ankle with bilateral full-thickness plantar burns (exit wounds).
On the way to hospital, the patient lost consciousness and became hemodynamically unstable. At the hospital, due to bilateral pneumothorax, chest tubes were inserted, and with suspicion of internal bleeding, exploratory laparotomy was done for the patient. After splenectomy and IVC repair, he was transferred to the ICU for a couple of days. During the immediate resuscitation, the patient underwent fasciotomy of left forearm for compartment syndrome decompression. By taking different X-rays, possible fractures were ruled out. Subsequently, the patient again was taken to the operating room where debridement of the left arm wound and the burned cortex of humerus was performed. The defect was covered by latissimus dorsi musculocutaneous island flap. Eighteen days later, the left ankle defect was reconstructed by reverse sural flap, and both plantar wounds were covered by split-thickness skin graft. He was discharged from hospital 45 days after admission to the Plastic Surgery ward.
On September 25, 2010 (about 18 months later), the patient was referred to the physician with complaints of a sudden severe left arm pain following a click-like sound after it was held by his friend in sitting position. Left arm radiographs showed a complete fracture and separation of two segments, in the mid shaft of humerus and another fracture in the proximal shaft. (Fig 1)
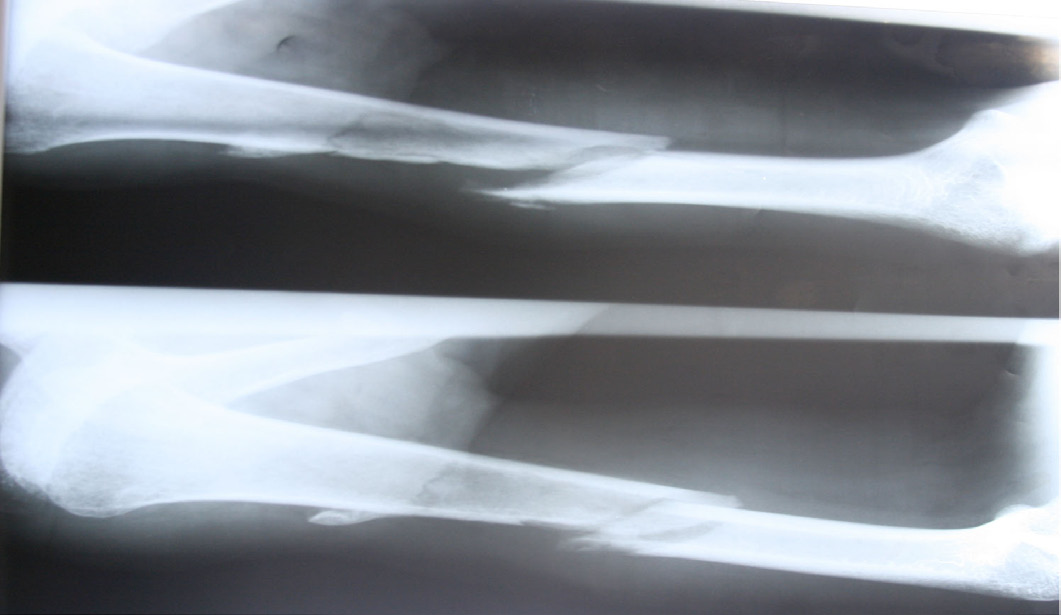
Figure 1: Humerus Fracture- 18 months after primary trauma.
So external splinting with bandage was applied to the patient for 4 weeks. The patient was visited two months later, where nearly complete union in the mid shaft fracture and incomplete union in the proximal part, with proper alignment were seen. (Fig. 2)
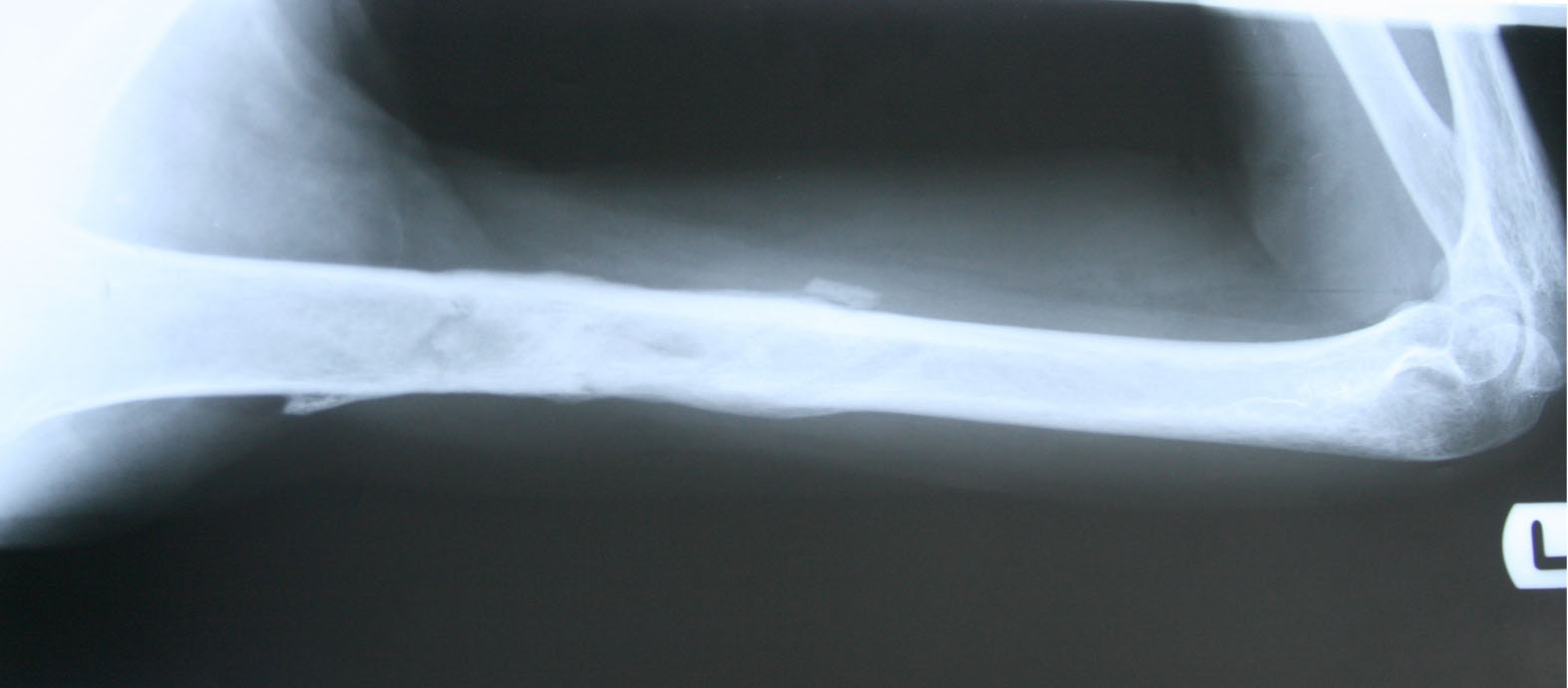
Figure 2: Follow-up figure which shows complete healing.
Two months later, the patient presented with a plantar wound with purulent discharge, and his foot roentgenogram showed erosion and complete destruction of the head of 4th metatarsal bone which was in favor of chronic osteomyelitis. After bone and soft tissue debridement and granulation tissue appearance, the skin graft was performed. (Fig. 3)
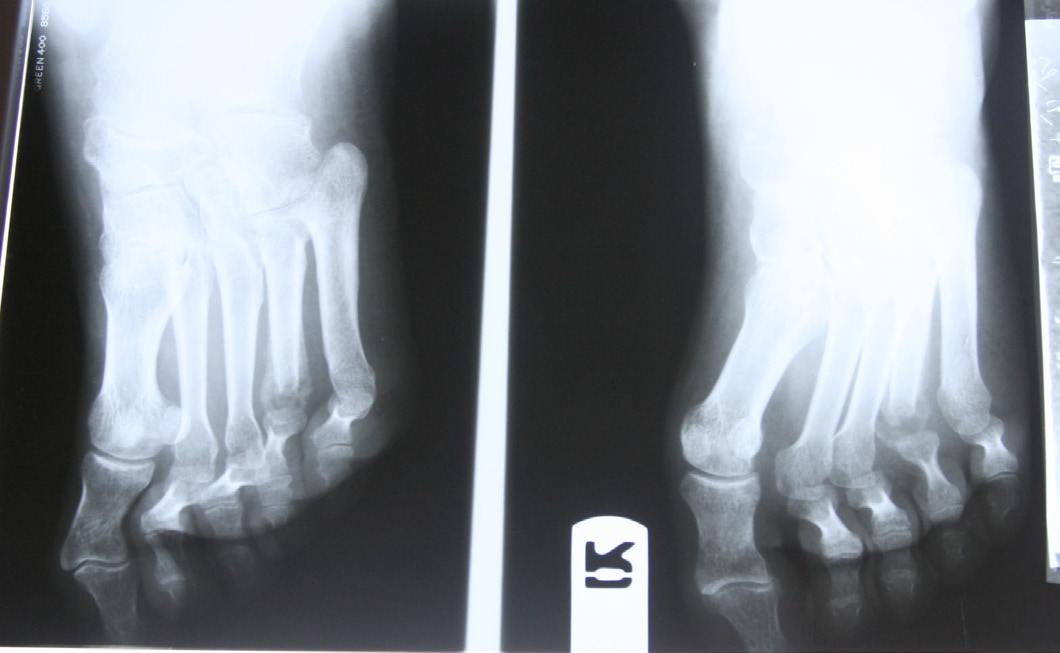
Figure 3: Foot roentgenogram which shows chronic osteomyelitis of the head of 4th metatarsal bone.
Discussion
Electrical injuries are relatively common which can result in tissue destruction and organ dysfunction. Electrical injuries can rarely cause skeletal system involvement, such as Long bone fractures, cervical spinal fractures, joint dislocations and heterotopic ossification of soft tissues. Because bone has the highest resistance of any body tissue, it generates the greatest amount of heat when exposed to an electrical current. Thus, the areas of greatest thermal injury are often the deep tissue surrounding long bones, resulting in periosteal burns, destruction of bone matrix, and osteonecrosis.7 Fractures usually occur early after a traumatic event due to electrical injuries, and only a few cases caused by violent tetanic muscle contractions the associated with electricity.8-10 The three sources of blood supply to the long bone should be mentioned as the main reason for low incidence of delayed fractures. The nutrient artery provides the principal source of blood supply to the marrow cavity and the inner cortex. The diaphyseal periosteal vessels supply the outer cortex of the diaphysis. The metaphyseal-epiphyseal periosteal vessels penetrate the cortex of the bone in the adult and anastomose with the nutrient artery, providing adequate supply to the marrow cavity and inner cortex in cases of disruption of the nutrient artery.11-13 In cases of high voltage injuries, the current will pass through the path between an entry and exit point and damage blood vessels, nerves and muscles.14,15 The resulting destruction is often difficult to diagnose at the time of initial debridement. Stripping of the devitalized periosteum and obtaining early soft tissue coverage limits the magnitude of bony injury.10
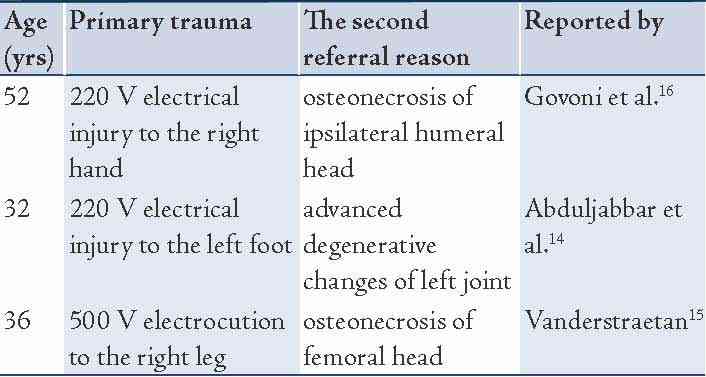
Although examinations and radiographs of our patient during the first admission showed no fracture, he presented left humerus pathologic fracture 20 months later. Govoni et al. described a 52-year-old patient having osteonecrosis of ipsilateral humeral head following a 220V electrical injury to the right hand.16 Fahad et al. reported a case of a 32-year-old man who received 220V electrical injury to the left foot and has subsequently shown advanced degenerative changes of left joint with narrowing of the joint space and a diagnosis of osteonecrosis of femoral head was made.14 Vanderstraetan stated that a 500V electrocution to the right leg of a 36-year-old patient led to osteonecrosis of femoral head 18 months later.15 (Table 1)
Table 1: Previous osteonecrosis cases following electrical trauma.
In this case, passage of the high voltage current and direct trauma could destroy metaphyseal and medullary blood supply. Also, debridement of cortex and stripping of the periosteum can damage the periosteal system, the most significant source of blood supply during the early stages of fracture or bone repair.17 This possible process could be attributed to ischemia to the humerus and subsequent osteonecrosis, which could have made the patient in this case prone to the pathologic fracture 18 months later.
Conclusion
The patients who sustained high voltage, 4th degree electrical bone injuries and underwent reconstructive surgery seem to be susceptible to osteonecrosis and pathologic fractures, therefore, these patients should be under close follow-up, and periodic radiologic evaluations may be recommended.
Acknowledgements
The authors reported no conflict of interest and no funding was received for this work.
References
1. Mohammadi AA, Amini M, Mehrabani D, Kiani Z, Seddigh A. A survey on 30 months electrical burns in Shiraz University of Medical Sciences Burn Hospital. Burns 2008 Feb;34(1):111-113. Published online 6 Jul 2007.
2. Cheng PT, Lee CE, Yang JY. Electrical injury–clinical report of 67 cases. Changgeng Yi Xue Za Zhi 1994 Sep;17(3):220-225.
3. Nursal TZ, Yildirim S, Tarim A, Caliskan K, Ezer A, Noyan T. Burns in southern Turkey: electrical burns remain a major problem. J Burn Care Rehabil 2003 Sep-Oct;24(5):309-314.
4. Dzhokic G, Jovchevska J, Dika A. Electrical Injuries: Etiology, Pathophysiology and Mechanism of Injury. Macedonian Journal of Medical Sciences. 2008 Dec;1(2):54-58 .
5. Robin A. Hurley, L. Anne Hayman,, Katherine H. Taber. Electrical Injury, Part I: Mechanisms. J Neuropsychiatry Clin Neurosci 21:3, Summer 2009:240-244.
6. Lochaitis A., Parker I, Stavropoulou V., PanaVotaki D.NEUROLOGICAL DISORDERS FOLLOWING ELECTRICAL BURN INJURIES. Annals of the MBC - vol. 4 - n' 2 - June 1991
7. Jain S, Bandi V. Electrical and lightning injuries. Crit Care Clin 1999 Apr;15(2):319-331.
8. Tan AH. Missed posterior fracture-dislocation of the humeral head following an electrocution injury to the arm. Singapore Med J 2005 Apr;46(4):189-192.
9. Gehlen JM, Hoofwijk AG. Femoral neck fracture after electrical shock injury. Eur J Trauma Emerg Surg 2010 Oct;36(5):491-493.
10. ten Duis HJ. Acute electrical burns. Semin Neurol 1995 Dec;15(4):381-386.
11. Rhinelander FW. The normal microcirculation of diaphyseal cortex and its response to fracture. J Bone Joint Surg Am 1968 Jun;50(4):784-800.
12. Trueta J. Blood supply and the rate of healing of tibial fractures. Clin Orthop Relat Res 1974 Nov-Dec;(105):11-26.
13. Trueta J. The role of vessels in osteogenesis. J Bone Joint Surg Br 1963;45:402-418.
14. Fahad H. Abduljabbar,Mohammed J. Al-Sayyad.Osteonecrosis of the Femoral Head Triggered by an Electrical Injury.JKAU: Med. Sci., Vol. 16 No.3, pp: 93-98.
15. Vanderstraeten L, Binns M. Osteonecrosis of the femoral head following an electrical injury to the leg. J Bone Joint Surg Br 2008 Aug;90(8):1101-1104.
16. Govoni M, Orzincolo C, Bigoni M, Feggi L, Pareschi PL, Trotta F. Humeral head osteonecrosis caused by electrical injury: a case report. J Emerg Med 1993 Jan-Feb;11(1):17-21.
17. Rhinelander FW. Tibial blood supply in relation to fracture healing. Clin Orthop Relat Res 1974 Nov-Dec;(105):34-81.
|