|
Abstract
Objective: The aim of this study was to evaluate the trans-axillary surgical approach in patients with thoracic outlet syndrome.
Methods: This retrospective study is comprised of data acquired from January 1998 until Oct 2008. Case histories of all the patients were reviewed from the Medical Records Department of Sher-i-Kashmir Institute. Relevant information and follow-up of the patients was carried out by examining the relevant clinical notes available by telephone interviews and personal contact whenever possible. All data was compiled and analyzed statistically.
Results: There were a total of 139 patients. The female: male ratio was about 6:1. Pain was the most common presenting symptom followed by weakness and parasthesia. Nerve conduction velocity was abnormal in 111 patients. Twenty-eight patients had abnormal Doppler study of subclavian vessels. Preoperative symptoms persisted in 13 patients. Overall, 126 patients showed improvement in symptoms and no recurrence or persistence of symptoms on follow-up examination.
Conclusion: Trans-axillary approach provides a good exposure and cosmesis in patients with thoracic outlet syndrome. It should be considered as the gold standard in the management of thoracic outlet syndrome.
Keywords: Trans-axillary; Cervical rib; Pain.
Introduction
Thoracic outlet syndrome is a clinical entity which produces a symptom complex with a myriad of presentations, caused by compression of neurovascular structures as they leave the thoracic cage through its upper aperture. There are three major clinical manifestations: Neurogenic type - it is predominant, accounting for 90 to 95% of all patients; Arterial type - accounts for less than 5% and results from compression of the subclavian artery; Venous type - it is uncommon and results from thrombosis of the subclavian or axillary vein, and usually occurs due to some sort of trauma.
The basic anatomical factor responsible for compression is the displaced anatomy to which congenital, traumatic and occasionally atherosclerotic factors may contribute. X-ray cervical spine and determination of nerve conduction velocities (NCV) is a widely used test in the diagnosis. Once the diagnosis is established, a course of conservative therapy should be instituted prior to consideration of surgical intervention.
Methods
This retrospective study is comprised of data acquired from January 1998 until October 2008. Case histories of all the patients were reviewed from Medical Records Department of Sher-i-Kashmir Institute. Relevant information and follow-up of the patients was carried out by examining the relevant clinical notes available, through telephone interviews and personal contact wherever possible. All patients were subjected to X-ray cervical spine AP and lateral view, Color Doppler study of subclavian vessels and nerve conduction velocity of upper limbs. All patients with cervical rib were operated by the trans-axillary approach. Transverse incision was made below the hairline between the Pectoralis major anteriorly and the latissimus dorsi muscle posteriorly, then deepened to the external intercostals fascia. The insertion of the scalenus anticus muscle on the first rib was dissected and the muscle was divided. The first rib was dissected subperiosteally and the cervical rib was excised, if found. Any abnormal band or bony spur were also excised. Postoperatively, patients were clinically assessed for persistent symptoms. Patients were discharged after 3 days to one week. After the first week, Doppler study of the subclavian vessels was performed for assessment of blood flow. Nerve conduction velocity study was repeated to assess any improvement after 3 weeks interval, and this was repeated every 3 months if abnormal. All the data was compiled and analyzed statistically.
Results
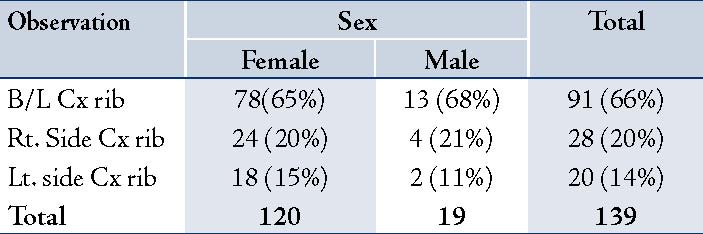
There were a total of 139 patients. The female: male ratio was about 6:1. Median age was 28 years old. Right limb involvement was seen in 55 (40%) patients, left side in 47 (34%) patients and bilateral upper limb was involved in 37 (27%) patients. Pain was the most common presenting symptom followed by weakness and parasthesia. Also, 127 (91%) patients had pain in the affected limb at the time of presentation (Table 1). Cervical spine X-ray AP and lateral revealed bilateral cervical rib in 91 patients, right side cervical rib in 28 patients and left side cervical rib in 20 patients (Table 2). Nerve conduction velocity was abnormal in 111 patients as shown in Table 3. Only 28 patients had normal NCV, while 52 patients had decreased conduction velocity or delay in latency in the ulnar nerve. In addition, 48 patients had involvement of both ulnar and median nerve, while median nerve involvement without ulnar nerve involvement was seen in 6 patients. Associated radial nerve conduction abnormality was evident in 5 patients. Also, 28 patients had abnormal Doppler study showing decreased flow in the subclavian vessels. After diagnosis, all the patients were subjected to surgery under general anesthesia through the trans-axillary approach.
Table 1: Symptoms - Sex Cross Tabulation.
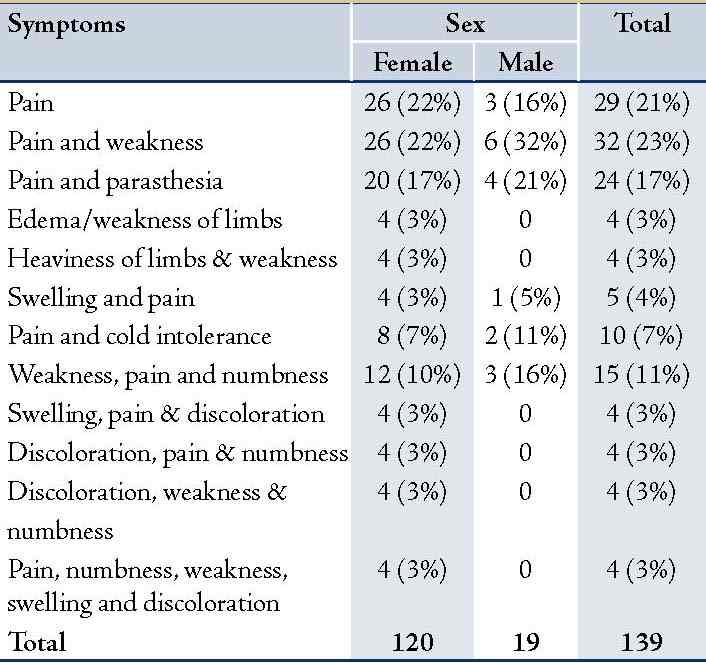
Table 2: X-Ray Cx Spine - Sex Cross Tabulation
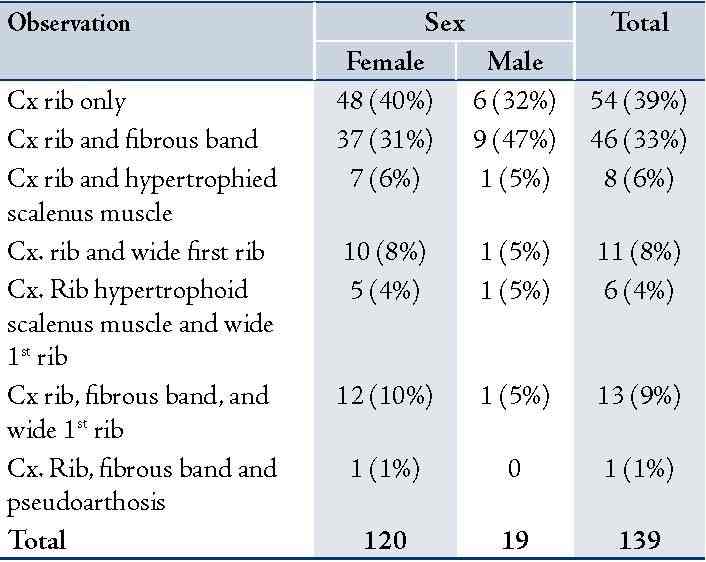
All patients had a Cx. Rib. Fifty patients (36%) had associated fibrous band extending between Cx. Rib and first rib. The results also showed that 19.4% of patients had wide first rib and 8.6% had hypertrophic scalenous muscle. One patient (1%) had pseudorthosis of Cx. Rib, and one patient (0.7%) had operative injury to the brachial plexus. This patient required regular analgesia, physiotherapy and was followed-up for 1 year. On one year follow-up, the patient still complained about parasthesia, loss of sensation in the arm supplied by C8,T1, and weakness in the small muscle of the hand. Operative findings in patients were noted. (Table 4)
Table 3: Nerve Conduction - Sex Cross Tabulation.
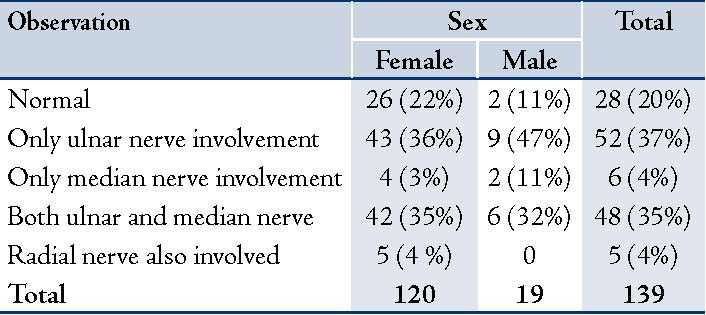
Table 4: Operative Findings - Sex Cross Tabulation.
Preoperative, symptoms persisted in 13 patients. Eight of them had bony prominence evident on Cx spine X-ray in postoperative period and was assumed to be responsible for post-operative persistence of symptoms. One-hundred and twenty-six patients had shown improvement in symptoms and showed no recurrence or persistence of symptoms on follow-up exam. Out of 111 patients who had abnormal NCV preoperative, 8 continued to have delay in NCV on post-operative follow-up. Out of 28 patients who had abnormal Doppler study (subclavian vessel compression), only 2 confirmed to have delay in flow on subclavian vessels on hyperabduction during postoperative follow-up.
Discussion
Thoracic outlet syndrome (TOS) refers to a compression of one or more of the neurovascular structures traversing the superior aperture of the chest. Previously, the name was designated according to the etiologies of compression, such as scalenus anticus, costoclavicular, hyperabduction, cervical rib, or first rib syndromes. Peet coined the term "thoracic outlet syndrome" in 1956 to designate compression of the neurovascular bundle at the thoracic outlet.1 The presence of a cervical rib is not always clearly related to the syndrome. Since cervical ribs can be observed in 0.5-1% of the general population, only 10% of these patients presented with symptoms. There are fibromuscular ligaments in 98% of patients with TOS. These ligaments have been found to exist in 33% of cadavers not having TOS. These findings suggest a congenital predisposing reason for most TOS cases.2 The emergence of symptoms upon the congenital predisposing factors in the second to third decade seems to be related to minor or major traumas, the pain-spasm vicious cycle, excessive muscular activity with myotendinitis and body posture. In fact, TOS cases form two groups according to these reasons. The first group consists of the people with extensive muscle development in the arm and shoulder regions. The second group consists of asthenic people. The patients in the second group respond well to regulation of the upper thorax posture towards normal and physical therapy.3 The most frequent clinical feature of TOS is pain in the affected upper limbs, followed by weakness, numbness and parasthesia. Pain and parasthesia were the most frequently observed symptoms in approximately 95% of patients in the study conducted by Sanders et al.4
All patients had a cervical rib on X-ray. Fifty patients (36%) had associated fibrous band extending between the cervical rib and the first rib, 19% of patients had wide first rib, and 9% had hypertrophic scalene muscle. One patient had pseudo-orthosis of the cervical rib. In a study by Brown and Charlesworth, they showed that all the patients in their study had cervical rib, 78% had complete cervical rib, and 22% of the patients had incomplete cervical rib.5 Reilly et al. have presented the findings of wide first rib in 2% of patients in their studies.6 While a study by Balci et al. revealed that the most frequent cause of thoracic outlet syndrome was cervical costae (40%).7
One patient in this study had brachial pluxes injury, but none of the patients had pneumothorax or vascular injury. Complication rate of 22% has been reported by DeGeorges et al.8 Although in a study by Altobell et al. they recorded a total complication rate of 4%, pneumothorax in 2% of the patients, 1% with vessel injury and 1% with nerve injury.9
Thirteen patients (9%) had postoperative recurrence or persistence of symptoms. Ambrad-Chalela et al. identified that in 6% of patients, incomplete first rib resection was responsible for the symptomatic recurrence and that incomplete excision of the first rib is an occasional cause of thoracic outlet syndrome recurrence.10 Conversely Mingoli A. et al. reported that a long first rib posterior stump shown by routine follow-up CXR film was responsible for thoracic outlet syndrome recurrence in 80% of cases.11 Adel Abdellaoni et al. concluded in their study that 82% of patients had complete resolution of symptoms,12 while 18% of the patients had poor outcome following thoracic outlet syndrome in the series conducted by Geven et al.13
Axelrod et al. concluded that more than 90% of patients reported improvement in both pain and paresthesia during short term follow-up examination and 66% of patients improved symptoms on long term follow-up examination.14 Brown and Charlesworth in their study concluded that 9% of patients had recurrence or persistent symptoms.5 In this study, out of 28 patients who had subclavian artery compression preoperatively, 2 patients (1%) showed persistence with decreased flow in the subclavian vessel on Color Doppler with improvement in 99% of patients following surgical decompression. Out of 111 patients who had decreased nerve conduction velocity, only 8 (7%) had postoperative abnormal nerve conduction velocity. In the study conducted by Balci et al.15 all patients had improvement of NCV except for 1 patient (2%).
Conclusion
Trans-axillary approach provides a good exposure and cosmesis in patients with thoracic outlet syndrome. It should be considered as the gold standard in the management of thoracic outlet syndrome.
Acknowledgements
The authors reported no conflict of interests and no funding was received for this work.
References
1. Peet RM, Henriksen JD, Anderson TP, Martin GM. Thoracic-outlet syndrome: evaluation of a therapeutic exercise program. Proc Staff Meet Mayo Clin 1956 May;31(9):281-287.
2. Sheth RN, Belzberg AJ. Diagnosis and treatment of thoracic outlet syndrome. Neurosurg Clin N Am 2001 Apr;12(2):295-309.
3. Athanassiadi K, Kalavrouziotis G, Karydakis K, Bellenis I. Treatment of thoracic outlet syndrome: long-term results. World J Surg 2001 May;25(5):553-557.
4. Sanders RJ, Hammond SL. Management of cervical ribs and anomalous first ribs causing neurogenic thoracic outlet syndrome. J Vasc Surg 2002 Jul;36(1):51-56.
5. Brown SC, Charlesworth D. Results of excision of a cervical rib in patients with the thoracic outlet syndrome. Br J Surg 1988 May;75(5):431-433.
6. Reilly LM, Stoney RJ. Supraclavicular approach for thoracic outlet decompression. J Vasc Surg 1988 Sep;8(3):329-334.
7. Balci AE, Balci TA,Cakir O, Eren S, Eren MN. Surgical Treatement of Thoracic outlet syndrome:effect and results of surgery. Ann Thorac Surg 2003; 75:1-91-96.
8. Degeorges R, Reynaud C, Becquemin JP. Thoracic outlet syndrome surgery: long-term functional results. Ann Vasc Surg 2004 Sep;18(5):558-565.
9. Altobelli GG, Kudo T, Haas BT, Chandra FA, Moy JL, Ahn SS. Thoracic outlet syndrome: pattern of clinical success after operative decompression. J Vasc Surg 2005 Jul;42(1):122-128.
10. Ambrad-Chalela E, Thomas GI, Johansen KH. Recurrent neurogenic thoracic outlet syndrome. Am J Surg 2004 Apr;187(4):505-510.
11. Mingoli A, Feldhaus RJ, Farina C, Cavallari N, Sapienza P, di Marzo L, et al. Long-term outcome after transaxillary approach for thoracic outlet syndrome. Surgery 1995 Nov;118(5):840-844.
12. Abdellaoui A, Atwan M, Reid F, Wilson P. Endoscopic assisted transaxillary first rib resection. Interact Cardiovasc Thorac Surg 2007 Oct;6(5):644-646.
13. Geven LI, Smit AJ, Ebels T. Vascular thoracic outlet syndrome. Longer posterior rib stump causes poor outcome. Eur J Cardiothorac Surg 2006 Aug;30(2):232-236.
14. Axelrod DA, Proctor MC, Geisser ME, Roth RS, Greenfield LJ. Outcomes after surgery for thoracic outlet syndrome. J Vasc Surg 2001 Jun;33(6):1220-1225.
15. Balci AE, Balci TA, Cakir O, Eren S, Eren MN. Surgical treatment of thoracic outlet syndrome: Effect and results of surgery. Ann Thorac Surg 2003; 75:1-91-6.
|