| |
Abstract
Objective: To describe the etiology, clinical presentation, management and outcome of liver abscess in adult patients admitted at Hamad general hospital, Qatar.
Methods: A cross sectional study was conducted to involve all adult patients who sequentially encountered episodes of liver abscess during the period from January 1, 2009, to December 31, 2010. Blood cultures were drawn from all patients in the first 24 hours after admission. In addition, all patients had stool examinations and indirect Hemagglutination test for Entameba histolytica. Aspiration of abscess was done under CT guidance and aspirated pus was sent for gram stain and culture.
Results: In total, 67 patients were admitted with liver abscess; 56 patients with pyogenic liver abscess and 11 with amebic liver abscess. There were 61 (91%) males and six (9%) females and their mean age was 47.4 ± 18.5 years. Fever, abdominal pain and vomiting were the commonest presenting features. Of the 56 pyogenic liver abscess patients, four discharged against medical advice and seven refused all invasive procedures and were treated with antibiotics for six weeks. The remaining 44 (79%) patients were treated with antibiotics and one or more invasive procedures, while one patient was treated surgically. The commonest organism isolated was Klebseilla pneumonia found in 21 patients (38%). The mean duration of hospitalization was 13.6 ± 8.1 days; the mean duration of antibiotic therapy was 34.7 ± 40.6 days, and one patient died. In contrast, all amebic liver abscess patients underwent ultrasound guided aspiration and showed good response to metronidazole treatment. Their mean duration of hospitalization was 7.7 ± 4.1 days, mean duration of therapy was 11.8 ± 2.1 days, and all patients were cured.
Conclusion: Pyogenic liver abscess was more common than amebic liver abscess with Klebseilla pneumonia being the commonest organism. With good medical measures and early drainage of liver abscess, surgical intervention was unnecessary in almost all the cases.
Keywords: Liver abscess; Amoebic abscess; Pyogenic abscess; Klebseilla pneumonia.
Introduction
Liver abscess remains an important clinical problem with a significant mortality rate in both developing and developed countries. It could result as a complication of various intra-abdominal infections; by hematogenous spread via portal vein from the gastrointestinal tract; or, may develop after traumatic injury to the liver. The two most common varieties of liver abscess are pyogenic and amoebic.1 Amoebic liver abscess is an important cause of space-occupying lesions of the liver; mainly in developing countries accounted for 3-9% of all cases of amoebiasis.2 This infection is caused by the protozoa E. histolytica, which ascends the portal venous system. Liver abscesses are the most common type of visceral abscess; in one study of intraabdominal abscesses, pyogenic liver abscesses accounted for 48% of visceral abscesses and 13% of intraabdominal abscesses.3 The annual incidence of pyogenic liver abscess has been estimated at 2.3 cases per 100,000 populations and is higher among men than women (3.3 vs. 1.3 per 100,000).4-6
Liver abscess is a common medical problem in Qatar; its exact incidence is unknown. This study is the first report of liver abscess among adult patients in Qatar. The aim of this study was to describe the etiology, clinical presentation, management and outcome of liver abscess among patients admitted to Hamad general hospital, Qatar.
Methods
This is a cross sectional study, conducted at Medical department in Hamad general hospital, which is a tertiary center of more than 600 beds. The study involved all adult patients (>15 years old) and it was designed to include all sequentially encountered episodes of liver abscess during the period from January 1, 2009, to December 31, 2010.
Blood cultures were drawn from all patients in the first 24 hours after admission. Two sets of blood were collected for culture from two different venipuncture sites as well as a single set of blood cultures consisted of aerobic and anaerobic samples. In addition, all patients had stool examinations and indirect Haemagglutination test for Entameba histolytica. Aspiration of abscess was done under CT guidance and aspirated pus was sent for gram stain and culture.
A pyogenic liver abscess was defined as a hepatic lesion demonstrated at Ultrasound (US) and/or computed tomography (CT) in a patient with a compatible clinical picture (various combinations of features of sepsis, right upper quadrant pain, and abnormal liver function), plus one or more of the following: (a) a positive culture result from aspiration of the lesion, (b) a positive blood culture result, or (c) clinical response to antibiotic treatment. On the other hand, amoebic liver abscess was defined as a hepatic lesion demonstrated at US and/or CT-scan in a patient with a compatible clinical picture (various combinations of features of sepsis, right upper quadrant pain, and abnormal liver function), plus one or more of the following: (a) recovery of amebas from the aspirate, (b) recovery of hematophagous trophozoites of Entameba histolytica from the stool, or (c) a positive amoebic serology of more than 1:256 by indirect hemagglutination test according to our laboratory reference, with clinical response to antiamoebic treatment.
From January 1, 2009, to December 31, 2011, all patients with liver abscess were identified in a prospective way: daily checks of hospital admissions, microbiology laboratory were made. All patients in the study gave signed consent and data were collected on a standard form that included demographic characteristics, clinical presentation of liver abscess, risk factors of liver abscess, coexisting medical conditions, laboratory tests (i.e. microbiological culture from blood and/or aspirate, stool examination, amebic serology), type of imaging study, abscesses characteristics (i.e., site, size and numbers of abscesses), type of interferences and duration of admission. The choice of interventions was delegated to the consultants in charge of the patient’s treatment. The patients were examined daily for clinical improvement. Improvement in pain, fever, anorexia and hepatomegaly were considered criteria for successful treatment.
Quantitative variables were expressed as mean ± SD. Student t test was used for continuous variables. Fisher exact and Chi Square tests were used to compare data in different groups. Results were considered significant if the p value was less than 0.050. Statistical analysis was carried out using the software package SPSS version 17.0 (SPSS, Inc., Chicago, IL, USA).
Results
During the study period, 67 patients were admitted to the hospital with liver abscess; sixty one (91%) patients were males and 6 (9%) were females. The mean age of all patients (±SD) was 47.4 ± 18.5 years (range: 21-106 years). In all, 58 (87%) of patients were non-Qatari and 9 patients were Qatari. A total of 56 (91%) patients had pyogenic liver abscess, whereas 11 (9%) patients had amebic liver abscess. Mean duration of symptoms before presentation in all cases was 8.4 day and the average hospital stay was 12.8 days.
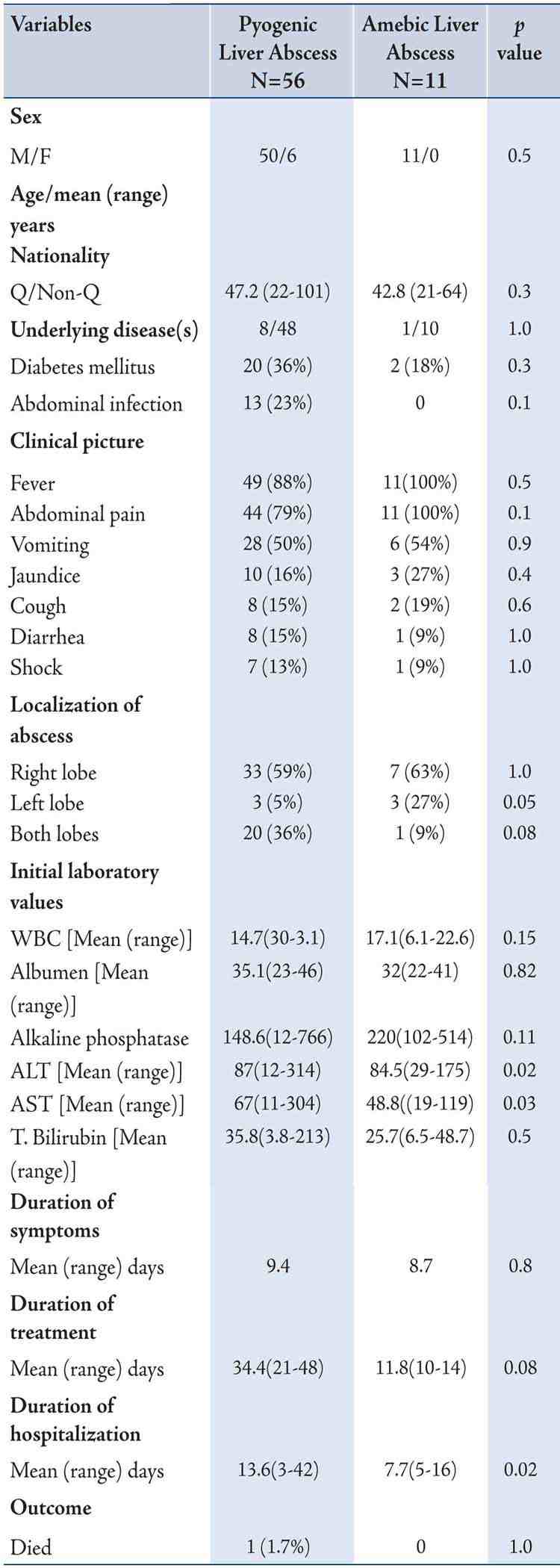
A total of 56 patients were admitted with pyogenic liver abscess; the mean age of them was 47.2 years. Forty eight cases occurred in non-Qatari residents, whereas eight cases occurred in Qatari. Twenty patients (36%) had diabetes and 13 (23%) had abdominal infection. Mean duration of symptoms was 9.4 ± 9.1 day (range of 1-30 days) with fever being the most frequent symptom noted in 49 (88%) patients. Abdominal pain was found in 44 (79%) patients. Table 1 summarizes the clinical profile of patients with liver abscess. A single lesion in right hepatic liver was found in 33 (59%) patients, while multiple lesions were found in 20 (36%) patients and only three (5%) patients had the abscess in left hepatic lobe.
Table 1: Demographic and clinical characteristics of patients with pyogenic and amoebic liver abscess.
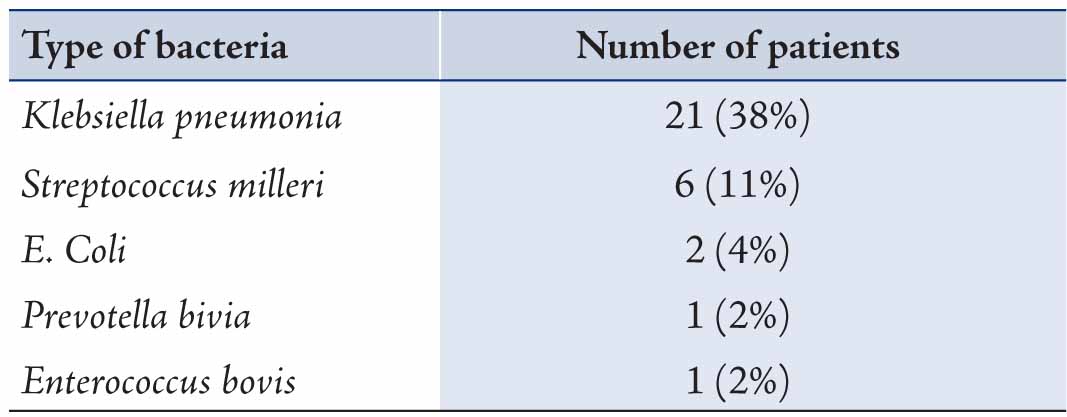
Seven patients (13%) were treated solely with antibiotics as they refused the invasive procedures. Their blood cultures were negative and they responded to 14-day intravenous antibiotics and discharged on oral antibiotic for another four weeks. Other four (7%) patients were discharged against medical advice and they left the country; their blood cultures also were negative. The remaining 44 (79%) patients were treated with antibiotics and one or more invasive procedures (aspiration and/or drainage), while one (2%) patient was treated surgically. Thirty one patients had positive blood and/or abscess aspirate cultures. The most common organism isolated was Klebseilla pneumonia found in 21 (36%) patients, followed by Streptococcus melleri in 6 (11%) patients, E. coli in two (4%) patients, Prevotella bivia and Enterococcus bovis in one (2%) patient each (Table 2). The mean duration of hospitalization was 13.6 ± 8.1 days, and the mean duration of antibiotic therapy was 34.7 ± 40.6 days. One patient died.
Table 2: Microbiology of pyogenic liver abscess.
Of the 67 patient in this study, 11 patients were admitted with amebic liver abscess and all of them were males. The ages ranged between 21 and 64 years (mean age of 42.8 years). Two patients (18%) were diabetic and fever was the most common finding at presentation, occurring in all patients. Mean duration of symptoms was 8.7 ± 4.4 day (range: 3-21 days). Table 1 summarizes the clinical profile of patients with liver abscess. Seven patients (64%) had one abscess in the right hepatic lobe and three patients (27%) had one abscess in the left hepatic lobe while one patient (9%) had multiple hepatic abscess. All patients with amebic liver abscess underwent ultrasound guided aspiration and showed good response to metronidazole treatment. Tests for Entameba histolytica were negative in aspirated materials and there were no bacterial isolates. The mean duration of hospitalization was 7.7 ± 4.1 days, and the mean duration of therapy was 11.8 ± 2.1 days. All patients were cured and there were no mortalities.
A comparison has been made between pyogenic and amoebic liver abscesses. There were no significant differences with respect to sex, age and clinical presentation. Patients with pyogenic abscess have higher liver enzymes than those with amoebic liver abscess. Table 1, describes the differences between patients with pyogenic and amoebic liver abscess.
Discussion
Liver abscess is one of the most important clinical problems confronting a physician in Qatar. The two most common varieties of liver abscess (pyogenic and amebic) are usually indistinguishable clinically and further investigations and/or invasive procedures are usually needed to establish the diagnosis as they have different lines of treatment. Contrary to previous reports,4,7,8 we found pyogenic liver abscess was more common than amebic, which may be attributed to improved socioeconomic condition in this country. Our observations are consistent with prior reports in many aspects. We noted similar presenting symptoms with fever, abdominal pain and vomiting being the common presenting features and there was male and right hepatic lobe predominance.1,2,4-7,9 Of note, the mean age of the population in this study (47.4 ± 18.5 yrs) was younger than that of other reports, which shows an upward shift in age range.5,7,10,11 The reasons for this are obscured but can be explained partially by Qatar and other Gulf countries having large working communities composed mainly of temporarily immigrant, predominantly Asian, unaccompanied young males.
In our series, as well as in other reports,7 the most common underlying condition was diabetes mellitus. Diabetes mellitus was more commonly associated with pyogenic abscess (37%) than with amoebic abscess (17%). Diabetic patients are particularly susceptible to metastatic foci.12 The reason is not well understood, but poor glycemic control leading to impaired neutrophil phagocytosis is thought to play a role.13 K. pneumoniae has emerged as the most common organism seen in pyogenic liver abscess in the Asian population, while in western countries K. pneumoniae accounted for about a quarter of all cases of pyogenic liver abscesses.14-16 In our study the most common isolated organism was k pneumonia. We did not note associated endophthalmitis, meningitis, or other serious metastatic infections as has been reported from other countries.12,15
It would seem that ultrasonography by an experienced radiologist should be the first line imaging modality in patients with suspected liver abscesses. CT scanning may confirm the ultrasonographic diagnosis, or make it, if the ultrasound is normal in the face of a high level of clinical suspicion. We found both these techniques to be reliable in the diagnosis and follow-up of the abscesses. Ultrasonography is less costly but the results are operator-dependent. The role of other imaging technique remains undefined. The distinction between pyogenic and amoebic liver abscess is difficult clinically and even by these imaging studies. Thus, further investigations might be needed to differentiate between them. The differentiation of amoebic from a pyogenic liver abscess is greatly assisted by amoebic serology, since laboratory tests like liver function tests and stool microscopy are non-discriminatory, facilities for culture are lacking and the positivity rate of bacterial culture (aspirate and/or blood) is only found in around 50% of the cases.8,17 Pyogenic abscesses must be excluded by pus aspiration and culture and sensitivity.18 In the present study, there were no significant differences between these two entities, except for significant high liver enzymes that were found in pyogenic liver abscess. (Table 1)
Majority of patients with pyogenic liver abscesses could be successfully managed by image guided aspiration / drain insertion with appropriate antibiotics treatment. Open surgical drainage infrequently required and the duration of antibiotics therapy is from 4-6 weeks. In the present study, 44 (79%) patients were treated with antibiotics and one or more invasive procedures (aspiration and/or drainage), while one patient was treated surgically. On the other hand, most uncomplicated amoebic liver abscesses can be treated successfully with amebicidal drug therapy alone. Consider therapeutic aspiration of amebic liver abscess in the following situations: a) high risk of abscess rupture, as defined by cavity size greater than 5 cm; b) left lobe liver abscess, which is associated with higher mortality and frequency of peritoneal leak or rupture into the pericardium; c) failure to observe a clinical medical response to antibiotic therapy within 5-7 days; and d) cannot differentiate from a pyogenic liver abscess.19 In our series, all patients with amebic liver abscess underwent ultrasound guided aspiration and showed good response to metronidazole therapy.
The overall mortality rate among pyogenic abscess group in our series (2%) is lower than the previously reported rate,4-7,9 this may be attributed to the age of our patients which was relatively younger than many reports.
Some limitations can be noted in our study; firstly, the study was hospital-based rather than population-based. However, our center is the only referral center in Qatar and therefore is likely to provide a true reflection of the actual burden of liver abscess in the country. Secondly, the number of cases was small.
Conclusion
The most common cause of liver abscess in the present study was pyogenic and among pyogenic liver abscess Klebsiella pneumonia was the commonest organism. With good medical measures, safe and aseptic drainage of liver abscess, surgical intervention was unnecessary.
Acknowledgements
The authors reported no conflict of interests and no funding was received for this work.
References
1. Cheema HA, Saeed A. Etiology, presentation and management of liver abscesses at the Children’s Hospital Lahore. Annals 2008;14:148-150.
2. Zafar A, Ahmed S. Amoebic liver abscess: a comparative study of needle aspiration versus conservative treatment. J Ayub Med Coll Abbottabad 2002 Jan-Mar;14(1):10-12.
3. Altemeier WA, Culbertson WR, Fullen WD, Shook CD. Intra-abdominal abscesses. Am J Surg 1973 Jan;125(1):70-79.
4. Huang CJ, Pitt HA, Lipsett PA, Osterman FA Jr, Lillemoe KD, Cameron JL, et al. Pyogenic hepatic abscess. Changing trends over 42 years. Ann Surg 1996 May;223(5):600-607, discussion 607-609.
5. Mohsen AH, Green ST, Read RC, McKendrick MW. Liver abscess in adults: ten years experience in a UK centre. QJM 2002 Dec;95(12):797-802.
6. Kaplan GG, Gregson DB, Laupland KB. Population-based study of the epidemiology of and the risk factors for pyogenic liver abscess. Clin Gastroenterol Hepatol 2004 Nov;2(11):1032-1038.
7. Yeoh KG, Yap I, Wong ST, Wee A, Guan R, Kang JY. Tropical liver abscess. Postgrad Med J 1997 Feb;73(856):89-92.
8. Lodhi S, Sarwari AR, Muzammil M, Salam A, Smego RA. Features distinguishing amoebic from pyogenic liver abscess: a review of 577 adult cases. Trop Med Int Health 2004 Jun;9(6):718-723.
9. Yu SC, Ho SS, Lau WY, Yeung DT, Yuen EH, Lee PS, et al. Treatment of pyogenic liver abscess: prospective randomized comparison of catheter drainage and needle aspiration. Hepatology 2004 Apr;39(4):932-938.
10. Sharma N, Sharma A, Varma S, Lal A, Singh V. Amoebic liver abscess in the medical emergency of a North Indian hospital. BMC Res Notes 2010;3:21.
11. Rintoul R, O’Riordain MG, Laurenson IF, Crosbie JL, Allan PL, Garden OJ. Changing management of pyogenic liver abscess. Br J Surg 1996 Sep;83(9):1215-1218.
12. Lee SS, Chen YS, Tsai HC, Wann SR, Lin HH, Huang CK, et al. Predictors of septic metastatic infection and mortality among patients with Klebsiella pneumoniae liver abscess. Clin Infect Dis 2008 Sep;47(5):642-650.
13. Lin JC, Siu LK, Fung CP, Tsou HH, Wang JJ, Chen CT, et al. Impaired phagocytosis of capsular serotypes K1 or K2 Klebsiella pneumoniae in type 2 diabetes mellitus patients with poor glycemic control. J Clin Endocrinol Metab 2006 Aug;91(8):3084-3087.
14. Pope JV, Teich DL, Clardy P, McGillicuddy DC. Klebsiella pneumoniae liver abscess: an emerging problem in North America. J Emerg Med 2011 Nov;41(5):e103-e105.
15. Wang JH, Liu YC, Lee SS, Yen MY, Chen YS, Wang JH, et al. Primary liver abscess due to Klebsiella pneumoniae in Taiwan. Clin Infect Dis 1998 Jun;26(6):1434-1438.
16. Rahimian J, Wilson T, Oram V, Holzman RS. Pyogenic liver abscess: recent trends in etiology and mortality. Clin Infect Dis 2004 Dec;39(11):1654-1659.
17. Ahsan T, Jehangir MU, Mahmood T, Ahmed N, Saleem M, Shahid M, et al. Amoebic versus pyogenic liver abscess. J Pak Med Assoc 2002 Nov;52(11):497-501.
18. Khan R, Hamid S, Abid S, Jafri W, Abbas Z, Islam M, et al. Predictive factors for early aspiration in liver abscess. World J Gastroenterol 2008 Apr;14(13):2089-2093.
19. e medicine: http://emedicine.medscape.com/article/183920-treatment#a1128 accessed on 15/5/2012.
|