The prescription of sickness certification is frequently practiced by general practitioners in primary health care. Between 11% and 35% of medical visits have been estimated to end with sickness certification.1 More than 60% of general practitioners reported having consultations that included consideration of sickness certification (SC) six or more times per week.2 Nevertheless, certifying sickness leave is not an easy task.3 General practitioners experienced a number of barriers to what they perceived to be good sick-listing practice.4 Moreover, sickness absence is a burden to national economy of any country. For example, sickness absence cost an average of £595 per employee during 2013 in the United Kingdom.5
At least 145 countries provide paid sick days for illnesses, with at least 81 countries providing sickness benefits for at least 26 weeks or until recovery.6 The regulations in Oman are no exception. Omani labor law states: “An employee whose sickness is proved shall have the right to a sick leave not exceeding in total ten weeks in one year whether such weeks are continuous or separate.”7 Similarly, Omani civil law states that a sick employee is entitled to leave which is determined by a competent medical authority.8
The rate of SC varies between countries and this may be a reflection of different certification policies.9,10 Sickness absence has been studied thoroughly in developed countries with the associated social, occupational, psychiatric, and medical issues explored. A look at the trends in Oman regarding SC in primary health care has not been published to date.
Estimation of the SC rate and describing associated medical and occupational factors are vital to provide solid data for future policies. In addition to being a global measure of health differentials between workers, sickness certification might give important prognostic data for chronic conditions.11,12
The primary health services in Oman are widely distributed. By 31 December 2013 there were 195 governmental health centers all over the country and 31 of these were in Muscat.13 Almost all these health centers use an electronic medical record system (EMRS).14 It is well known that EMRS has the advantage of preventing duplication to workups and other services.15 All prescribed SC are recorded in the EMRS for each patient.
This study aimed to determine the rate and trend of SC issued in the Bowsher province in Oman by using the electronic data retrospectively to describe associated demographic, medical, and occupational factors.
Methods
This cross-sectional study reviewed the data of all SC from four health centers, which were retrieved retrospectively from EMRS. The study was approved by the Research and Ethics Committee at Directorate General of Health Services in Governorate of Muscat. We included all consultations that ended with SC between 1 January 2011 and 31 December 2011. Consultations of patients aged less than six years old and more than 65 years old were excluded.
The study was conducted in the Bowsher province, which is part of Muscat Governorate. Bowsher is located in central area of the capital city, Muscat. It hosts 365,284 people of whom about 80,982 are native Omanis.16 Primary health care is delivered through four governmental health centers scattered through the region.
The operating EMRS in these health centers is the A’Shifa system. Each patient has a single medical record number containing their demographic characteristics, clinical consultations data, and SC. All clinical consultations that end with sickness certification are documented in the system. Each certificate includes information about the diagnosis, designation, issuing date and time, and the duration of leave given. These are filled by the doctor conducting the consultation during the visit.
These data was analyzed using Microsoft Excel and statistics performed using SPSS software. Examined variables included: gender, age, nationality, occupation, clinical diagnosis, and duration of sickness absence. Suitable rates were calculated as percentages and important differences were compared using the chi-square test.
Each consultation with sickness certification had a diagnosis given according to the International Classification of Diseases (ICD-9). All consultations were screened to determine the most common diagnosis. The patients’ designations were recorded by the general practitioner at the time of prescribing the sickness certification for each consultation. All designations were retrieved from the EMRS and categorized into public, private, school, and college work sectors, and if the written designation was ambiguous it was categorized as unknown.
The SC rate was calculated as the number of all certificates issued, divided by the total number of visits in 2011. The crude rate was presented as a percentage. Specific rates for each health center, age categories, gender, and designation were calculated in similar way with the nominator being of similar category.
Results
The total number of consultations for all patients aged six to 65 years old in 2011 was 189,275 out of which there were 26,096 SC issued for 15,758 patients. The minimum and maximum prescribed off-days were 1 and 14, respectively. The overall rate of SC was 13.8 per 100 consultation-years (ie. 13.8 sick leaves per 100 consultations per year; CI 13.6–14) which represents a frequency of one sickness certification per seven consultations. The rate was significantly higher in males (13,721/79,017; 17 per 100 consultation-years) in comparison to females (12,536/110,248; 11 per 100 consultation-years) with a p-value of less than 0.001. This was universal in the four health centers. Most SC (n=24,916; 95%) were prescribed for Omanis and the rate was significantly higher among this group (14 per 100 consultation-years) compared to non-Omanis (9 per 100 consultations/year) with a p-value <0.001.
To study association between SC and age, we divided age into 10-year intervals as follows: <19, 19–29, 30–39, 40–49, and 50–65 years. The SC rates were found to be 15.7, 18.6, 16.1, 7.7, and 3 per 100 consultation-years in these age groups, respectively. The difference in the SC rates was significant between all age groups with the exception of the first and third group where there was no difference. The highest rate of SC was found among the 19–29 age group and lowest among 50–65 age group with p-value <0.001 [Figure 1]. More specifically, calculated rate of SC was 20 per 100 consultations per year for people aged 25–29 years old.
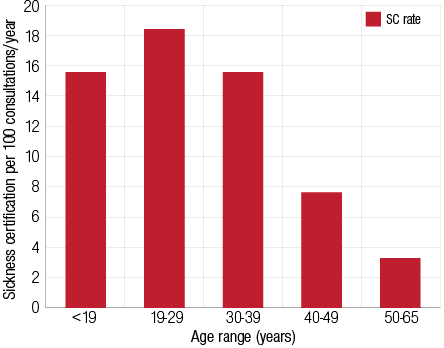
Figure 1: Sickness certifications (SC) rate according to age group. The sickness certification rate was highest among youth and peaked in 19–29 year old age group.
Figure 2 illustrates most frequent ten diagnoses which represent (17101/25463; 67%) of all diagnosis for SC. In this group of patients, the highest proportion of certification was for acute respiratory infections.
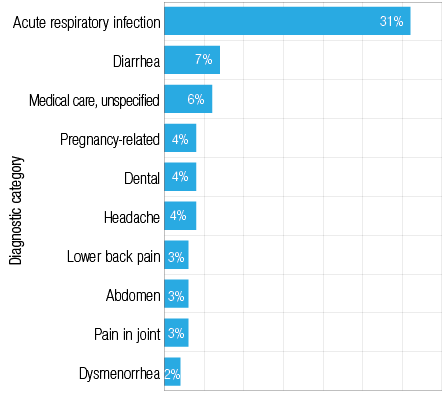
Figure 2: The 10 most frequent diagnosis categories of sickness certifications. Respiratory tract infection was the most frequent diagnosis followed by diarrhea and medical care, un-specified.
Based on designation record of 14,826 patients, 28% and 11% of patients who were prescribed SC were school and college students, respectively. Workers in the private and public sectors composed 24% and 22% of certified patients, respectively. About 15% of patient occupations could not be identified. Total absence due to sick leave for patients aged 19–65 years old in 2011 was 28,491 days.
In addition, 30% (n=7,800) of certificates were issued without any of the vital signs being documented. Finally, the highest rates of SC during 2011 were in October (3,317/19,787; 17%) followed by March (2,993/18,488; 16%) and the lowest were in August (927/10,215; 9%) and July (1,294/13,648; 9%) [Figure 3].
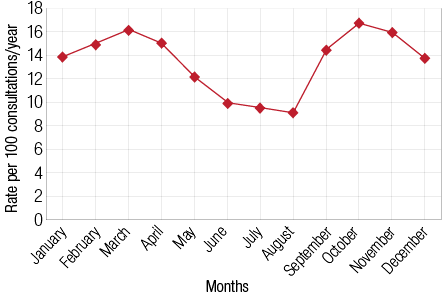
Figure 3: Total rate of sickness certifications per months during 2011. The highest certification was in March and October. The summer months reported the lowest rates.
Discussion
This was descriptive study of sickness certification practice in primary health care. Sickness absence does not merely represent lost working days and productivity but also reflect patients’ morbidity and pressure on health system.5,17 Although variation between countries in national rates of SC is known,9,10 the rate reported in this study is high.
In medical literature, the rates are often calculated by patients-years rather than consultation-years. We choose the later because it provides a better reflection of the clinical and workload burden. Calculating sickness certification rate per 100 consultations per year describes how frequently sick leaves is issued by general practitioners. The prescription of sick leave is part of the daily practice of general practitioners in primary health care. This study reported that among 100 consultations per year, 13.8 ends with a certification of sick leave. Many qualitative studies have showed that issuing sick leave is a burden on general practitioners daily work and carries many challenges with each encounter.3,18 The high patient demand of sickness certification might affect the quality of clinical consultations and overall performance of clinical system.
Calculation of the rate based on all consultation dilutes it and makes it lower than actual rate, and this is a limitation of the study. Even with this limitation, the rate remains high with a general frequency of one every seven consultations in the four health centers ending with SC. Another limitation is not including sick leave prescribed by private clinics in Bowsher. There are many private clinics and hospitals that are also authorized to give SC. However, most of these prescriptions are written manually and not registered, documented, or reported in an electronic system and are therefore difficult to trace.
In a Swiss prospective study, Sebastien Dunner et al,19 reported that 11 per 100 consultations resulted in SC during a six-week period. The relatively small sample size, the total 602 sick leaves included in statistical analysis, and the short period of the study makes comparison with our study inappropriate. In addition, the Swiss sick leave benefit system is different and allows workers to get self-certification of sickness absence for up to three days.
The rate of certification was highest in young adults between 19–29 years and more specifically in 25–29 year age group [Figure 1], among whom one in five consultations are estimated to end with sickness certification. This high rate could not be explained by increased morbidities because people in this age group are usually viewed to be healthier than others. A recent study from the United Kingdom reported the highest rate of certifications in the 45–49 year old age group.20 Excluding children younger than the age of four, people aged 20–29 years old represent highest percentage of the total Omani population according to National Center of Statistics and Information,16 although this does not explain higher rate of sickness absence.
These figures might demonstrate a huge burden on the economy especially with an estimated 28,491 lost working days over a one-year period, and from only four health centers. In Oman, workers are paid in full while on sick leave for up to six months.8
Many medical literatures determined that mental and musculoskeletal conditions were the most common reason for certifying sickness absence, especially for a long duration.20,24 In this study, respiratory tract infections were the most frequent diagnosis followed by diarrhea and medical care, un-specified. This last diagnosis sounds broad and non-specific, but because of the large sample size tracing each consultation classed as medical care, un-specified was not feasible.
Many studies showed sickness absence to be higher in women.9,20,21 Our study clearly showed that males were significantly more likely to take sick leave in comparison to females, and this was universal in the four studied health centers. Out of every six clinical consultations with male patients, one ended with sickness certification. This discrepancy may be attributed to fact that males are more often employed than females especially in the private sector.16 However, the employment gap between the two genders decreased dramatically over the past decade and this difference in the sick leave certification rate should be investigated more.22,25 Work satisfaction and job strain also has a role in patients seeking sickness certification, and this idea can be explored by further studies in the Omani population.25,26
The decision to prescribe sick leave should be based on robust clinical evaluation. Vital signs were not found in about one third of sickness certification visits. This could be either because they were not documented appropriately or were not performed at all. Student’s leave made up more than one quarter of all SC. Added to college students leave this made up around 40% of total certifications. Sick leave regulation should be set within teaching institutions, colleges, and schools in order to decrease the pressure on health centers, minimize unnecessary absence, and to organize the process of sickness certification.
Categorization of government or private sector worker sick leave was not optimal due to poor designation identification in about 15% of working patients. This suggests the need for better documentation.
Monthly variation of SC presented well in this study [Figure 3]. The rate was lowest during summer months: June, July, and August and peaked during March and October. This is likely due to people taking holidays during the summer and consequently demand of sickness certification decreases especially by colleges and schools students.
Sickness certification is a complex practice and further investigations are needed to determine the risk factors leading to the high rate found in this study, especially among young people. Health care recommendations should be based on best available research27 and results of this study should provide an evidence for future sick leave prescriptions policy.
Conclusion
Sickness certification represents a burden on primary health care in the studied health centers with approximately one in seven consultations ending with SC. Young people and males are more likely to be prescribed sick leave certifications. Respiratory tract infection was the most frequent diagnosis leading to SC. Further research to identify determinates of high sickness absence is needed. Robust guidelines are also needed to regulate the sickness certification.
Disclosure
The authors declared no conflicts of interest. No funding was received for this work.
Acknowledgements
The authors extend deep appreciation to Mr Jaseer Kalathiyath for his cooperation in data collection for this study. We also thank Dr Sulaiman Al-Shukaili for advice regarding methodology and data analysis.
references
- Tellnes G. Sickness certification in general practice: a review. Fam Pract 1989 Mar;6(1):58-65.
- Löfgren A, Hagberg J, Arrelöv B, Ponzer S, Alexanderson K. Frequency and nature of problems associated with sickness certification tasks: a cross-sectional questionnaire study of 5455 physicians. Scand J Prim Health Care 2007 Sep;25(3):178-185.
- Kiessling A, Arrelöv B. Sickness certification as a complex professional and collaborative activity–a qualitative study. BMC Public Health 2012;12:702.
- Swartling MS, Alexanderson KA, Wahlstrom RA. Barriers to good sickness certification–an interview study with Swedish general practitioners. Scand J Public Health 2008 Jun;36(4):408-414.
- Chartred Institute of Personnel and Development. Absence Management: Annual survey report 2013. p18.
- Heymann J, Earle A, Hayes J. 2007. The Work, Family and Equity Index: How Does the United States Measure Up? Institute for Health &Social Policy, 2007.
- Oman. 2003. Omani Labour Law. Royal Decree 2003/35, Chapter 4, Article 66.
- Oman. 2004. Omani Civil Law. Royal Decree 120/2004, Chapter 10, Article 72.
- Barmby TA, Ercolani MG, Treble JG. Sickness absence: an international comparison. Econ J 2002 June;112(480):F315-F331.
- Wynne-Jones G, Mallen CD, Welsh V, Dunn KM. Rates of sickness certification in European primary care: a systematic review. Eur J Gen Pract 2008;14(3-4):99-108.
- Kivimäki M, Head J, Ferrie JE, Shipley MJ, Vahtera J, Marmot MG. Sickness absence as a global measure of health: evidence from mortality in the Whitehall II prospective cohort study. BMJ 2003 Aug;327(7411):364.
- Kivimäki M, Head J, Ferrie JE, Singh-Manoux A, Westerlund H, Vahtera J, et al. Sickness absence as a prognostic marker for common chronic conditions: analysis of mortality in the GAZEL study. Occup Environ Med 2008 Dec;65(12):820-826.
- Ministry of Health. Oman. Annual Health Report 2013, Directorate General of Planning, Department of Information and Statistics, 2014.
- Mohammed E, Al-Hosni A, Day K, Al-Hamadani A, Al-Toqi A, Al-Shamli N et al. Review of Health Information Systems in Oman. SQU Journal For Science, 2007; 12(2):101- 120.
- Ganesh A, Al-Mujaini A. Electronic Medical Record System: Have we Bitten off More Than we Can Chew? Oman Med J 2009 Jan;24(1):1-3.
- National Center for Statistics and Information. Statistical Year Book 2013. Issue 42: Section 2; page 8-9 Published 06/08/2014.
- Soler JK, Okkes IM. Sick leave certification: an unwelcome administrative burden for the family doctor? The role of sickness certification in Maltese family practice. Eur J Gen Pract 2004 Jun;10(2):50-55.
- Nilsing E, Söderberg E, Berterö C, Öberg B. Primary healthcare professionals’ experiences of the sick leave process: a focus group study in Sweden. J Occup Rehabil 2013 Sep;23(3):450-461.
- Dünner S, Decrey H, Burnand B, Pécoud A. Sickness certification in primary care. Soz.-Präventivmed. 2001:46:389-95.
- Wynne-Jones G, Mallen CD, Mottram S, Main CJ, Dunn KM. Identification of UK sickness certification rates, standardised for age and sex. Br J Gen Pract 2009 Jul;59(564):510-516.
- Allebeck P, Mastekaasa A. Swedish Council on Technology Assessment in Health Care (SBU). Chapter 5. Risk factors for sick leave—general studies. Scand J Public Health 2004;32(Suppl63):49-108.
- Omani women getting better education, taking up more jobs. From: http://www.timesofoman.com/News/Article-30884.aspx. Accessed March 10, 2013.
- 68,200 Omani women work in public sector. From: http://main.omanobserver.om/?p=62960. Accessed 9, 2014.
- Laaksonen M1. Pitkäniemi J,Rahkonen O,Lahelma E. Work arrangements, physical working conditions, and psychosocial working conditions as risk factors for sickness absence: Bayesian analysis of prospective data. Ann Epidemiol 2010 May;20(5):3328.
- Renée Bourbonnais, Myrto Mondor. Job strain and sickness absence among nurses in the province of Québec. American Journal of Industrial Medicine 39(2): 194–202.
- Magee C, Stefanic N, Caputi P, Iverson D. Occupational factors and sick leave in Australian employees. J Occup Environ Med 2011 Jun;53(6):627-632.
- Al-Riyami A. Health researchers and policy makers: a need to strengthen relationship. Oman Med J 2010 Oct;25(4):251-252.