| |
Introduction
Laparoscopic splenectomy is an acceptable approach for elective splenectomy in Hematological conditions. Nevertheless, the anatomical location, several ligamentous attachments, friability of the splenic tissue and intra-operative bleeding are the major challenges faced by Laparoscopic surgeons. To meet these challenges, many approaches are in practice for splenic mobilization and control of vascular pedicle. Newer advances such as; ultracision, ligasure devices, endostaplers and hand assisted ports have all facilitated this complex operation. Intra-operative bleeding remains the main cause for conversions to open surgery. Several authors have shown that preoperative embolization or ligation of the splenic vessels reduces the intra-operative bleeding and conversion rate. The ligation of the splenic artery is a routine practice in conventional elective open splenectomy prior to mobilization of the spleen. We maintained the same general approach and ligated the splenic artery prior to mobilization of the spleen to avoid intra-operative bleeding. Intra-operative bleeding is the main cause of conversion in laparoscopic splenectomy. Several studies have shown that early ligation of the splenic artery before mobilization of the spleen decreases the likelihood of bleeding and the conversion rate. Furthermore, it also decreases the blood loss during surgery, reduces the size of spleen and makes dissection and manipulation of this fragile organ easy. This study aims to show that elective intracorporeal ligation of the splenic vessels is safe and by reducing the bleeding and blood loss during surgery, it can facilitate laparoscopic splenectomy.
Methods
Between February 2002 and July 2009, laparoscopic splenectomy was attempted in 19 (>12 year old) consecutive patients. Open emergency splenectomies performed in trauma patients were not part of this study and were excluded.1 The medical notes were reviewed retrospectively. There were no elective open splenectomies performed during this period. Also, no controlled clinical or experimental arm was included for comparison. Seven patients were male and 12 were female, aged from 12-65 years (mean age of 33 years). Indications for splenectomy included idiopathic thrombocytopenic purpura (ITP), thalassemia major, idiopathic hypersplenism, and splenitis. (Table 1)
Table 1: Demography and results
| Diagnosis |
Pts. (n=19) |
| Idiopathic thrombolytic purpura |
14 |
| Thalassemia major |
3 |
| Splenitis |
1 |
| Idiopathic hypersplenism |
1 |
| Accessory spleen |
3 |
| Spleen size: |
|
| Normal (5x11 cm) |
13 |
| Moderate (>5x11 cm) |
3 |
| High grade (6x16 cm) |
3 |
| Mean spleen weight (gms) |
250 |
| Conversion rate |
- |
| Hand assist |
1 |
| Mean operation time (minutes) |
152 |
| Concomitant surgery |
5 |
| Mean blood loss |
45 |
| Transfusion |
1 |
| Complications |
6 |
| Mean hospital stay in days |
7 |
| Mean follow up in months (3-88) |
46 |
| Preoperative platelet count (109 per liter) |
15-45 |
| Postoperative platelet count (109 per liter) |
>300 |
| Accessory incision |
19 |
| Number of Trocar |
4 |
All patients were referred from the hematology department for splenectomy; ITP patients after failure of medical treatment and thalassemia major patients for hypersplenism, painful spleen and to reduce their transfusion requirements. The spleen was clinically enlarged in Thalassemia major patients, but in none of the ITP patients, while none had palpable spleen among the studied patients. Routine investigations included blood counts, liver and kidney function tests, coagulation profile, peripheral smear, and ultrasound of the abdomen. Platelet count varied from 15,000-45,000/ml and hemoglobin ranged between 7-11 g/dl on admission. Ultrasound showed moderate to high grade enlargement of the spleen in three ITP patients, three thalassemia major patients, and the rest had normal size.2 Two of the ITP patients had gall stones while one patient had hiatus hernia with significant reflux, and another ITP patient had bilateral inguinal hernia. The accessory spleen was not picked up in ultrasound in any of the patients.3 Bone marrow examination was done in one hypersplenism case. None of the patients had history of any prior abdominal surgery.
All patients received preoperative vaccinations of pneumococcal, hemophilus influenza and meningococcus vaccines two weeks prior to surgery, peri-operative antibiotic coverage was also administered. The ITP patients were managed on corticosteroids to improve the platelet count of over 50,000/ml pre-operatively, and doses of corticosteroids were gradually tapered postoperatively. All laparoscopic splenectomies were performed by the same consultant general surgeon proficient in laparoscopic surgery. Over 1000 therapeutic general surgical laparoscopic procedures were performed annually in this district hospital. Among these, the laparoscopic splenectomy was rather a rare operation. (It was difficult to set a minimum number of procedures needed in order to be accepted as proficient in this rather rare operation).
Informed consent was obtained from all patients. Laparoscopic splenectomy was performed using the anterior approach, thus patients were positioned in supine and modified lithotomy. The surgeons stood between the legs of the patient, this position and approach was appropriate for concomitant laparoscopic procedures. Pneumoperitoneum was established with Verres needle and carbon dioxide insufflated to a pressure of 13 mmHg. Trocars were placed along the left subcostal margin in epigastrium, midclavicular line and anterior axillary line under visual control. A 0° telescope was inserted through a 10 mm optical trocar in the left midclavicular line. (Fig. 1)
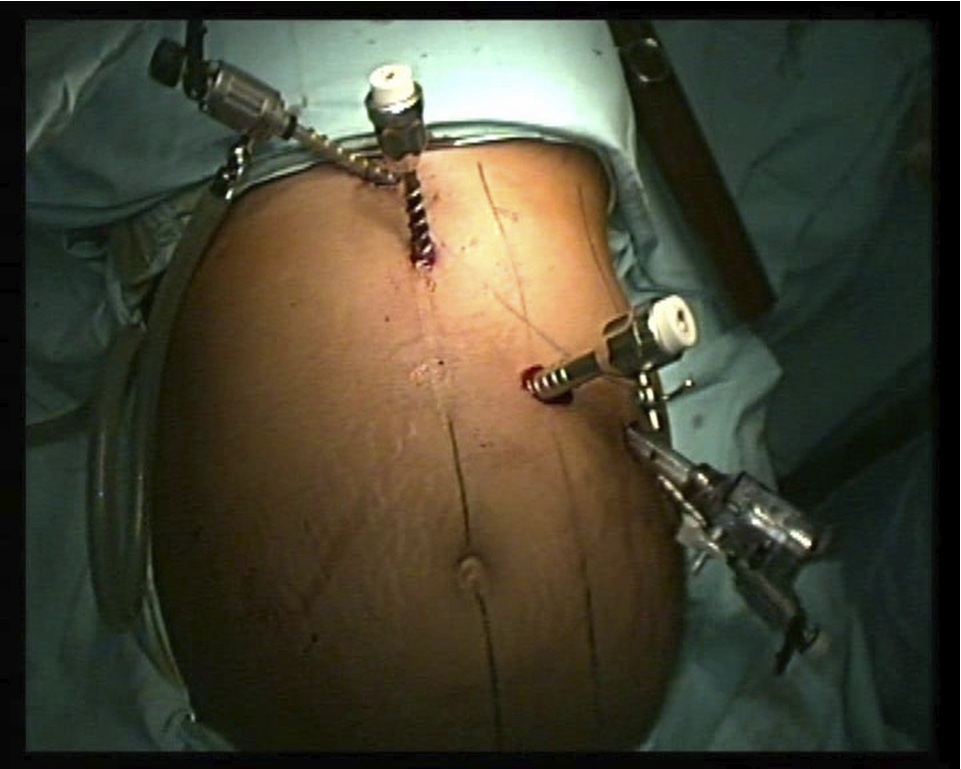
Figure 1: Port position.
An abdominal exploration was done to identify the accessory spleens near the hilum of the spleen, lesser sac, gastrolienal ligament and greater omentum, (Fig. 2). The anterior adhesions were cleared if present, and the anterior part of the spleen was exposed. The avascular area in gastrosplenic ligament was subsequently incised with ultracision and the lesser sac was opened.
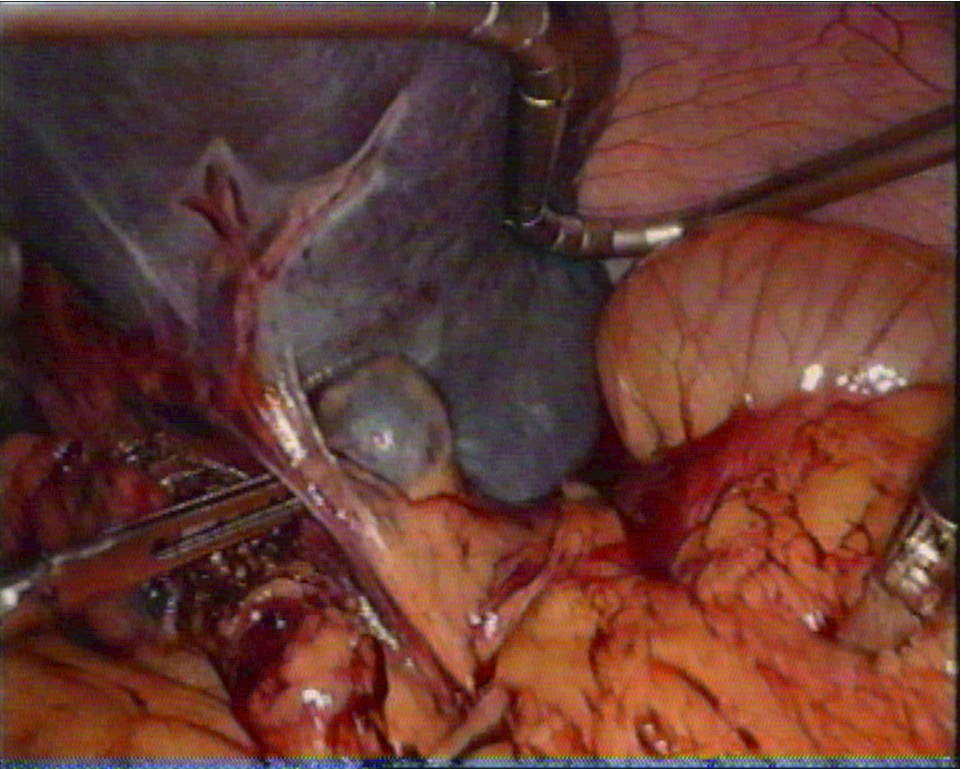
Figure 2: Accesory spleens near hilum of spleen.
The splenic artery was identified and dissected along the superior border of the pancreas in the lesser sac, and doubly ligated by intracorporeal knotting but not divided. (Fig. 3)
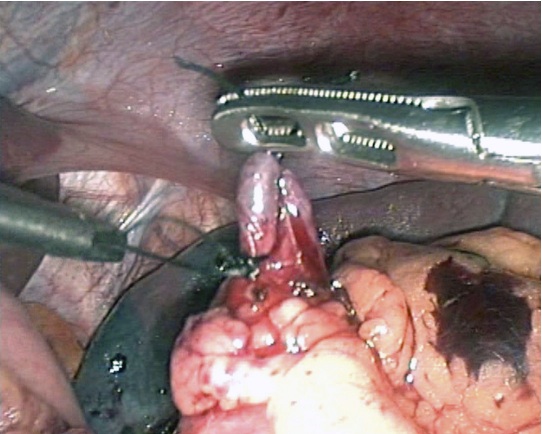
Figure 3: Splenic artery ligated in lesser sac.
The splenic vein which lies immediately beneath the artery was also isolated and a loose tie left around it but not tied at this stage, (Fig. 4). This practice allowed the spleen to shrink by draining the blood out, providing an auto trasfusion and made mobilization of the spleen easier later on. The gastrosplenic ligament and all short gastric vessels were further divided by ultracision forceps. The table was tilted to the right lateral position with reverse Trendelenburg for mobilization of the spleen. The lower pole of the spleen was mobilized next by dividing the splenocolic ligament to bring down the splenic flexure of the colon followed by the dissection of the posterior attachments (splenophrenic and splenorenal ligaments) with the help of ultracision. ( Fig. 5)
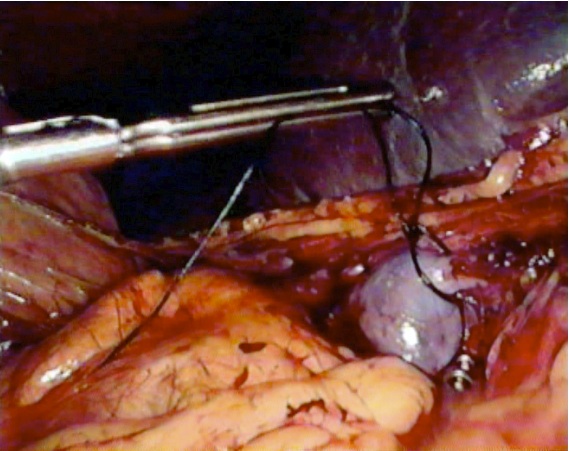
Figure 4: Loose tie around the splenic vein.
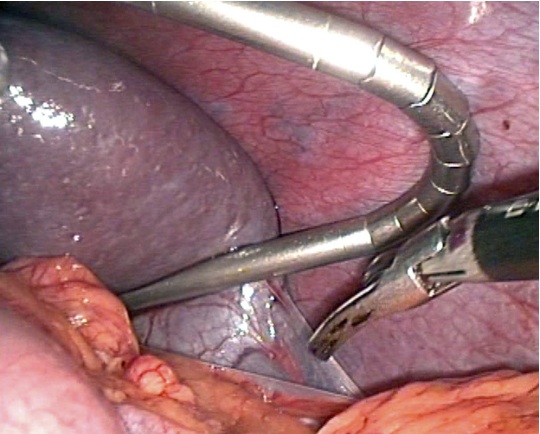
Figure 5: Lower pole of spleen mobolized by dividing splenocolic ligament using ultracision.
The splenic vein and artery were further tied proximally and distally and divided close to the hilum taking care of the pancreatic tail. Hemostatis was secured in the splenic bed. The spleen was placed in an airtight plastic bag (MTP medical technical single use extraction bag catalogue No. 040142-01) and removed through a short Pfannenstiel incision. (Fig. 6)

Figure 6: Spleen delivered in a plastic bag through 3-4 cm Pfannenstiel incision.
Larger spleens were removed by fragmenting in the plastic bag. The accessory spleens were dissected and removed separately. A suction drain was placed through the left lateral most port 10 mm. In patients with coexisting gall stones, hiatus hernia and inguinal hernia, laparoscopic cholecystectomy, Fundoplication and TAPP repair were performed respectively.
There was no conversion to open surgery but one patient had hand assisted splenectomy for a large spleen. There was no death, re- operation or wound infection. The operating time ranged from 140-273 minutes but with experience, it became less as in any surgery there is always a learning curve and laparoscopic splenectomy is no exception. Thus, the operative time improves with experience. Operation time was prolonged in patients with concomitant surgery.
Two patients underwent concomitant laparoscopic cholecystectomy for cholelithiasis, one patient had laparoscopic fundoplication for hiatus hernia with gastro esophageal reflux disease and one patient had laparoscopic repair of bilateral inguinal hernia repair.4 Also, two patients had the accessory spleen close to the hilum of the spleen and one had two accessory spleens. The weight of the spleens varied from 200-750 gms. The median estimated blood loss was 85 ml (ranging from 30-350 ml). Nasogastric tube and drains were removed on the first postoperative day and patients were allowed liquid to soft diet.
Laparoscopic splenectomy was successful in all patients except one had hand assisted splenectomy. The mean operating time was 152 minutes, mean hospital stay was 7 days and the mean estimated blood loss was 65 ml. One patient required blood transfusion during surgery, but none after surgery. There were no significant post-operative complications. In patients with idiopathic thrombocytopenic purpura, the platelet count improved greater than 300, 000 /ml after surgery. During follow up period of 12-97 months, there was one relapse in a patient of idiopathic thombocytic purpura after one year.
No significant post-operative complications occurred in any patient. Three patients had postoperative fever but all cultures were negative. Another two patients had minor left sided pleural effusion and one had minimal subphrenic collection. All complications were treated conservatively. One patient received blood transfusion and three patients had platelet transfusion a day prior to surgery. There was no evidence of any postoperative bleeding and no patient required postoperative blood or platelet transfusions. The median hospital stay was 8 days (ranging from 6-11 days). The stay in the hospital for the studied patients was longer compared to other studies. The majority of patients came from rural backgrounds and faraway places with no facilities to check their sequential platelet counts. We measured the platelet count on the 1, 3 and 7th postoperative days and then at three weeks. By then, the platelet counts usually peaked.
Early success (thombocytic count >150,000/L on 3rd postop. day) and late success was the same (thombocytic count >150,000/L on 3rd month). In patients with idiopathic thrombocytopenic purpura, the platelet count improved greater than 100 × 300/L after the surgery. The postoperative platelet counts exceeded over one million in five patients and were given oral aspirin as advised by a hematologist. There were no thrombo-embolic events. All patients were jointly followed in cooperation with a hematologist. In a follow-up period of 12-88 months, there was one relapse (platelet counts <50, 000/L) in a patient of idiopathic thombocytic purpura after one year, but extensive investigations in this patient did not show any evidence of accessory spleen and was managed by a hematologist. There was a complete response (platelet counts >150,000 /L without treatment) in 18 patients.5
Discussion
Laparoscopic splenectomy is becoming a standard approach in hematological conditions after a failed medical treatment.6-9 Better understanding of operative strategies, advances in instrumentations and increasing experience in laparoscopic surgery has produced results comparable to open surgery. Even a massive splenomegaly is not considered a contraindication to laparoscopy.10,11 However, it remains a technically challenging operation due to anatomical location and several ligament attachments of the spleen. The mobilization of this fragile vascular organ is difficult and leads to intra-operative bleeding, which is the main cause of conversion to open surgery.12 Several operative approaches are in practice to access the splenic vessels prior to mobilization of the spleen to minimize bleeding during surgery.13-18
Ligation of splenic vessels prior to splenic mobilization allowed partial emptying of the spleen, thus diminishing its size, facilitating auto transfusion, and decreasing the risk of hemorrhage as concluded by several authors.19-23 Asoglu et al. reported effective control of intraoperative bleeding with no extension of the operative time and low conversion rate during laparoscopic splenectomy with early ligation of the splenic artery before splenic lysis.20 Palanivelu et al. in their leaning spleen approach used the first elective arterial and secondary venal ligature to the preserved blood splenic sequestration.14 Indeed, ligation of the splenic artery has been used in children as a method to preserve the spleen in trauma.21 Xu et al. used CDFI (color Doppler flow imaging) in their study to standardize the ligation of the splenic artery. The splenic pedicle was ligated safely and quickly on the basis of anatomic information provided by preoperative CDFI.24 Even in a very large spleen of portal hypertension, early ligation was successful and saved conversion.25
Embolization of the splenic artery either preoperatively or intra- operatively has also been practiced to achieve the same desirable effects of ligation.26-32 Takahashi et al. with preoperative embolization of the splenic artery concluded its safety and considered it as a useful adjunct.28 While Naoum et al. evaluated the role of concomitant intraoperative splenic artery embolization in an effort to reduce the risk of bleeding and have shown reduced blood loss, operation time and conversion rate.29 Splenic artery embolization and injection of adrenaline into the splenic artery has been used in large spleens to reduce bleeding followed by splenectomy.
Operative strategy was dependent on the size of spleen and experience of the surgeon. We used the conventional anterior supine approach.33-37 The control of the splenic artery was straightforward in this approach in the lesser sac. We delayed the ligation of the splenic vein to reduce the risk of any significant bleeding. The use of ultracision shears in particular was very useful in maintaining a blood less field. Lagausie et al. in their anterior approach have shown elective splenic vessel endoligature in decubitus position was a better and safer approach than the other techniques. Other authors have found it convenient in lateral or posterior-lateral positions.14-16
Any further bleeding after ligation of vessels was minimal and usually secondary to splenic capsule tear and not a direct loss of blood. As in other laparoscopic procedures, where larger specimens were removed, the use of an accessory incision was well accepted and had advantages over the fully open approach. We have chosen infra- umbilical abdominal incision (Pfannenstiel) as this was usually less painful than supra-umbilical incision.
Conclusions
Compared to conventional open splenectomy, laparoscopic splenectomy enjoys the advantages of minimal access surgery of faster recovery, short hospital stay, less wound related and postoperative complications. The laparoscopic approach facilitated concomitant surgery and the intra-operative search for the accessory spleen. Our study showed that with early ligation of the splenic artery and delayed ligation of the splenic vein, there was minimal blood loss and bleeding during surgery and laparoscopic splenectomy was successful in all cases without conversion.
Thus, the practice of early ligation of splenic artery facilitated the laparoscopic splenectomy and decreased the chances of conversion to open surgery. Overall, Laparoscopic splenectomy should be considered as a procedure of choice in hematological conditions with normal size spleen. Furthermore, the success rate is high in expert hands with pre-emptive vascular control of the splenic vessels.
Acknowledgements
The author reported no conflict of interest and no funding was received on this work.
|
|
| |
1. Carobbi A, Romagnani F, Antonelli G, Bianchini M. Laparoscopic splenectomy for severe blunt trauma: initial experience of ten consecutive cases with a fast hemostatic technique. Surg Endosc 2010 Jun;24(6):1325-1330.
2. Görg C, Cölle J, Görg K, Prinz H, Zugmaier G. Spontaneous rupture of the spleen: ultrasound patterns, diagnosis and follow-up. Br J Radiol 2003 Oct;76(910):704-711.
3. Altaf AM, Sawatzky M, Ellsmere J, Bonjer HJ, Burrell S, Abraham R, et al. Laparoscopic accessory splenectomy: the value of peri-operative localization studies. Surg Endosc 2009;23:2675-2679.
4. Sasaki A, Nitta H, Otuska K, Kimura Y, Obuchi T, Wakabayashi G. Concomitant laparoscopic splenectomy and cholecystectomy. Surg Laparosc Endosc Percutan Tech 2010 Apr;20(2):66-68.
5. Supe A, Parikh M, Prabhu R, Kantharia C, Farah J. Post-splenectomy response in adult patients with immune thrombocytopenic purpura. Asian J Transfus Sci 2009 Jan;3(1):6-9.
6. Habermalz B, Sauerland S, Decker G, Delaitre B, Gigot JF, Leandros E, et al. Laparoscopic splenectomy: the clinical practice guidelines of the European Association for Endoscopic Surgery (EAES). Surg Endosc 2008 Apr;22(4):821-848.
7. Delaitre B, Champault G, Barrat C, Gossot D, Bresler L, Meyer C, et al; French Society of Laparoscopic Surgery. Laparoscopic splenectomy for hematologic diseases. Study of 275 cases. Ann Chir 2000 Jul;125(6):522-529.
8. Baccarani U, Terrosu G, Donini A, Zaja F, Bresadola F, Baccarani M. Splenectomy in hematology. Current practice and new perspectives. Haematologica 1999 May;84(5):431-436.
9. Schlinkert RT, Teotia SS. Laparoscopic splenectomy. Arch Surg 1999 Jan;134(1):99-103. PubMed doi:10.1001/archsurg.134.1.99
10. Targarona EM, Espert JJ, Balagué C, Piulachs J, Artigas V, Trias M. Splenomegaly should not be considered a contraindication for laparoscopic splenectomy. Ann Surg 1998 Jul;228(1):35-39.
11. Trelles N, Gagner M, Pomp A, Parikh M. Laparoscopic splenectomy for massive splenomegaly: technical aspects of initial ligation of splenic artery and extraction without hand-assisted technique. J Laparoendosc Adv Surg Tech A 2008 Jun;18(3):391-395.
12. Gossot D, Fritsch S, Célérier M. Laparoscopic splenectomy: optimal vascular control using the lateral approach and ultrasonic dissection. Surg Endosc 1999
Jan;13(1):21-25.
13. Trias M, Targarona E M, Balagu C. Laparoscopic splenectomy: an evolving technique. A comparison between anterior and lateral approaches, Surg Endosc (1996) 10: 389-392
14. Palanivelu C, Jani K, Malladi V, Shetty R, Senthilkumar R, Maheshkumar G. Early ligation of the splenic artery in the leaning spleen approach to laparoscopic splenectomy. J Laparoendosc Adv Surg Tech A 2006 Aug;16(4):339-344.
15. de Lagausie P, Bonnard A, Benkerrou M, Rorlich P, de Ribier A, Aigrain Y. Pediatric laparoscopic splenectomy: benefits of the anterior approach. Surg Endosc 2004 Jan;18(1):80-82.
16. Kuriansky J, Ben Chaim M, Rosin D, Haik J, Zmora O, Saavedra P, et al. Posterolateral approach. An alternative strategy in laparoscopic splenectomy. Surg Endosc 1998 Jun;12(6):898-900.
17. Wang KX, Hu SY, Zhang GY, Chen B, Zhang HF. Hand-assisted laparoscopic splenectomy for splenomegaly: a comparative study with conventional laparoscopic splenectomy. Chin Med J (Engl) 2007 Jan;120(1):41-45.
18. Dalvi AN, Thapar PM, Deshpande AA, Rege SA, Prabhu RY, Supe AN, et al. Laparoscopic splenectomy using conventional instruments. J Minim Access Surg 2005 Jun;1(2):63-69.
19. Stanek A, Stefaniak T, Makarewicz W, Kaska L, Podgórczyk H, Hellman A, et al. Accessory spleens: preoperative diagnostics limitations and operational strategy in laparoscopic approach to splenectomy in idiopathic thrombocytopenic purpura patients. Langenbecks Arch Surg 2005 Feb;390(1):47-51.
20. Asoglu O, Ozmen V, Gorgun E, Karanlik H, Kecer M, Igci A, et al. Does the early ligation of the splenic artery reduce hemorrhage during laparoscopic splenectomy? Surg Laparosc Endosc Percutan Tech 2004 Jun;14(3):118-121.
21. Keramidas DC, Soutis M. The function of the spleen in adults after ligation of the splenic artery of the traumatized spleen in childhood. Surgery 2003 May;133(5):583-585.
22. Schwalke MA, Crowley JP, Spencer P, Metzger J, Kawan M, Burchard KW. Splenic artery ligation for splenic salvage: clinical experience and immune function. J Trauma 1991 Mar;31(3):385-388.
23. Bessoud B, Duchosal MA, Siegrist CA, Schlegel S, Doenz F, Calmes JM, et al. Proximal splenic artery embolization for blunt splenic injury: clinical, immunologic, and ultrasound-Doppler follow-up. J Trauma 2007 Jun;62(6):1481-1486.
24. Xu WL, Li SL, Wang Y, Shi BJ, Li M, Li YC, et al. Laparoscopic splenectomy: color Doppler flow imaging for preoperative evaluation. Chin Med J (Engl) 2009 May;122(10):1203-1208.
25. Wang Y, Zhan X, Zhu Y, Xie Z, Zhu J, Ye Z. Laparoscopic splenectomy in portal hypertension: a single-surgeon 13-year experience. Surg Endosc 2010 May;24(5):1164-1169.
26. Iwase K, Higaki J, Yoon HE, Mikata S, Miyazaki M, Nishitani A, et al. Splenic artery embolization using contour emboli before laparoscopic or laparoscopically assisted splenectomy. Surg Laparosc Endosc Percutan Tech 2002 Oct;12(5):331-336.
27. Bau Plínio Carlos, Cavazolla Sílvio Adriano, Souza Hamilton Petry, Garicochea Bernardo. Preoperative embolization of the splenic artery in patients that underwent splenectomy for immune thrombocytopenic purpura. Acta Cir. Bras. 2007; 22(.6): 470-473 6
28. Takahashi T, Arima Y, Yokomuro S, Yoshida H, Mamada Y, Taniai N, et al. Splenic artery embolization before laparoscopic splenectomy in children. Surg Endosc 2005 Oct;19(10):1345-1348.
29. Naoum JJ, Silberfein EJ, Zhou W, Sweeney JF, Albo D, Brunicardi FC, et al. Concomitant intraoperative splenic artery embolization and laparoscopic splenectomy versus laparoscopic splenectomy: comparison of treatment outcome. Am J Surg 2007 Jun;193(6):713-718.
30. Poulin EC, Mamazza J, Schlachta CM. Splenic artery embolization before laparoscopic splenectomy. An update. Surg Endosc 1998 Jun;12(6):870-875.
31. Reso A, Brar MS, Church N, Mitchell P, Dixon E, Debru E. Outcome of laparoscopic splenectomy with preoperative splenic artery embolization for massive splenomegaly. Surg Endosc 2010 Aug;24(8):2008-2012.
32. Chen B, Hu SY, Wang L, Wang KX, Zhang GY, Zhang HF, et al. Laparoscopic splenectomy: a 12-year single-center experience. Chin Med J (Engl) 2008 Apr;121(8):766-768.
33. Barbaros U, Dinççağ A. Single incision laparoscopic splenectomy: the first two cases. J Gastrointest Surg 2009 Aug;13(8):1520-1523.
34. Malladi P, Hungness E, Nagle A. Single access laparoscopic splenectomy. JSLS 2009 Oct-Dec;13(4):601-604.
35. Kye BH, Park IS, Kim JG, Lee JC, Son GM, Suh YJ, et al. Laparoscopic splenectomy: 3 ports are enough. Surg Laparosc Endosc Percutan Tech 2010 Apr;20(2):104-108.
36. Targarona EM, Pallares JL, Balague C, Luppi CR, Marinello F, Hernández P, et al. Single incision approach for splenic diseases: a preliminary report on a series of 8 cases. Surg Endosc 2010 Sep;24(9):2236-2240.
37. Gagner M. Needlescopic splenectomy: a safer alternative to single incision laparoscopic splenectomy (SILS). J Gastrointest Surg 2010 Sep;14(9):1473.
|
|