|
A 61 years old woman with type II diabetes mellitus presented with fever, dysuria, reduced urine output and right flank pain since 5 days, not responding to treatment. There was no history of obstructive lower urinary tract symptoms, hematuria, or trauma. On examination, there was tenderness in the right flank. Laboratory tests revealed a white blood cell count (WBC) of 18,500/mm3 with 81% neutrophils, hemoglobin concentration of 9.7 g/dl, platelet count of 15,010/mm, creatinine level of 3.1 mg/dl and urea concentration of 118 mg/dl.
Urine analysis demonstrated a 20-25 WBC per high power field. Urine culture showed more than 105 colony-forming units (CFU) per mL of Escherichia coli (E.coli) sensitive to amikacin, ceftriaxone, ofloxacin, nitrofurantoin and trimethoprim. The patient’s abdominal X-ray is shown in Fig 1.
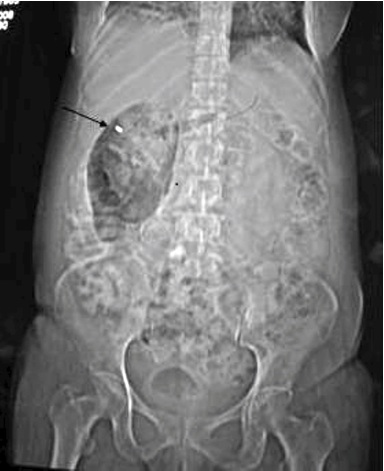
Figure 1: Abdominal X-ray supine view showing REINFORM shape collection of gas in right renal fossa (arrow)
Question
1. What is the diagnosis?
a. Loculated pneumoperitoneum b. Volvulus
c. Emphysematous pyelonephritis d. Toxic megacolon
e. None of the above
2. Which investigation to do next?
Answers
1. Emphysematous pyelonephritis
2. Computed tomography (CT) Abdomen
Discussion
Plain X-ray of abdomen showed a reniform shaped air collection in right renal fossa which was confirmed with CT Abdomen in our patient (Fig 2).
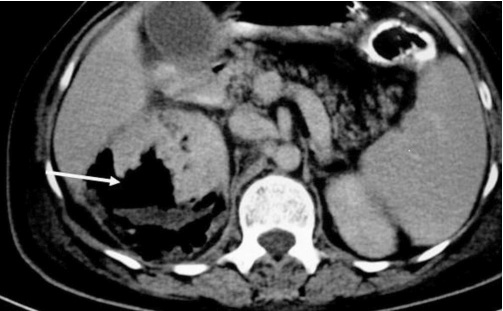
Figure 2: Contrast CT abdomen shows collection of air and fluid in renal parenchyma as well as perinephric space.
Emphysematous pyelonephritis (EPN) has been defined as a necrotizing infection of the renal parenchyma and its surrounding areas that results in the presence of gas in the renal parenchyma, collecting system or the perinephric tissue. More than 90% of cases occur in patients with diabetes. The factors that predispose to EPN in patients with diabetes are; poorly controlled diabetes, high levels of glycosylated hemoglobin A(1c), and local cause such as renal tract obstruction (tumors or lithiasis). E. coli and Klebsiella are the most commonly involved pathogens and mixed organisms are observed in 10% of the cases.1
Abdominal radiograph, Intravenous urography and ultrasound can detect EPN by demonstrating the presence of gas. Ultrasound demonstrates presence of multiple echogenic foci with dirty shadowing due to reverberation artifacts. However, gas within the kidney or renal pelvis can mimic renal calculi. Computerized tomography (CT) is the procedure of choice which is both a highly sensitive and a specific method for demonstrating intrarenal air and for characterizing the location and extent of that air (intracalyceal, intraparenchymal, perinephric, or pararenal), and thus planning the management. A CT classification of emphysematous pyelonephritis proposed by Wan et al. has prognostic significance.2
Two staging systems, based on CT findings, have been proposed for prognostic and therapeutic reasons. Wan et al. described two types. Type I- the classical form, includes patients showing parenchymal destruction with streaky or mottled gas but with no fluid collection. These patients have had a high mortality rate of 69%. Whereas, type II EPN is defined either as the presence of renal or perirenal fluid in association with a bubbly or loculated gas pattern, or gas in the collecting system with acute bacterial nephritis or renal or perirenal fluid-containing abscesses, which has a better prognosis than type I EPN.
Conclusion
The treatment of EPN remains controversial and nephrectomy is still the treatment of choice in severe cases. However, energetic management with more efficient antibiotics such as trimethoprim, cephalosporins, nitrofurantoin, or a fluoroquinolone, along with correction of fluid electrolyte imbalance, effective diabetic control and CT-guided percutaneous catheter drainage (PCD) of EPN was found to be a safe, quick and life-saving alternative to surgery, especially in type 2 EPN and in cases of single kidney or in an inoperable high-risk patient.3 But in cases of PCD failure, immediate nephrectomy should not be delayed for successful management of EPN.
Acknowledgements
The authors reported no conflict of interest and no funding was received on this work.
|